Circadian Rhythms & Temperature

Due to a bit of an erratic week, I haven't been able to reliably measure (and experiment with) my apnoeas, so instead this was going to be a blog post about "Circadian Rhythms" (the daily sleep/wake cycle).
Given that we inhabit a planet with a 24 hour day, it is no surprise that our bodies have become roughly linked with the day/night cycle, with various hormones being released at certain stages in the rhythm enticing us to sleep or wake.
(Combined photos from my Sky-Watcher and solar telescopes)
Not everyone's rhythm is the same, some people have theirs shifted (such as when you are jet lagged). Even a skew of an hour or two can make a huge difference to how easily you are able to wake up for work in the morning, or how late you can stay awake.
There are a couple of online questionnaires to help you determine your own circadian rhythm:
http://www.philips.co.uk/c/circadian/178344/cat/
http://www.bbc.co.uk/science/humanbody/sleep/crt/
Both of these decided that my rhythm was skewed, so I decided to make my own measurements and chart them here but after seeing the first 24 hours of data, something interesting emerged...
This is a normal circadian rhythm taken from the Philips website.
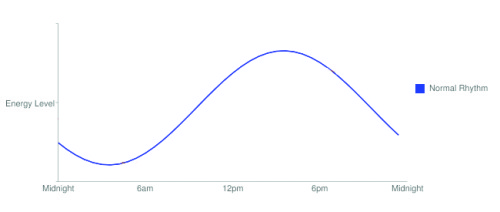
In fact, this is a simplified rhythm, because it is normal to have a small dip in the energy levels around mid afternoon, hence the reason for many countries having an afternoon siesta, and the reason why we tend to slump at our desks in the mid afternoon and reach for a cup of coffee.
This dip can be seen in my graph from the BBC circadian test.

Core body temperature is a good way of charting your own rhythm because energy levels are reflected by our temperature. Our body temperature is not a static 37.5 C, in fact it fluctuates throughout the day inline with our circadian rhythm. Of course, it is also affected by ambient temperature and how active we are.
So, all it would take to chart my own rhythm would be a decent thermometer.
I decided to get a data-logging thermometer, so that I could see what was happening while I was asleep.
I ordered a thermometer capable of recording every 10 seconds (to weed out anomalous readings), and was expecting the probe to be a small thermocouple-type sensor that I could stick to the skin under my arm, but the probe was more like a bullet and wasn't adhesive plus the logger turned out to be a lot bigger than it looked in the photo!
I'd gone this far, so in the name of science, I shaved under my arm and fixed the probe there with Melonin (low adhesive dressing) and Tegaderm (a clear waterproof adhesive dressing). I then wedged the cables into my suit and went off to work.
After 24 hours (and a few weird looks) I downloaded the data to a computer. I noticed that generally the pattern was the same as that belonging to "normal" people, but that it had a few fairly severe drops in temp during the night.
I repeated this over several days.
On the graph below, the dip is around 1:30pm and again at 4:00pm. I suspect the 1:30pm dip is my normal afternoon energy dip whilst the 4:00pm dip is environmental because I was working outside at 4:00pm.
I repeated this the following day and the dip was much more pronounced again early at around noon, but I ended the recording early as it was becoming awkward to carry the data-logger around with me, so I can't show a full 48 hour graph.
It's also interesting that the temperature drops around 8pm. That's pretty much when I start to look forward to sleep! It plateaus at 10pm for a couple of hours in a similar way to the one produced by my answers to the BBC link. This may have been because I was already asleep by then!
The first 24 hours...
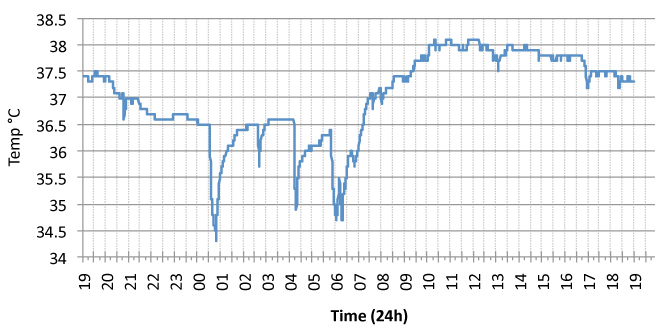
Those drops in temperature during sleep are severe. When I first saw them, I suspected that they were erroneous readings, but the probe was stuck so tightly to me that there was no way that these were due to poor contact (after all, if that were the case, why didn't this happen during the day when there was more movement?). However, as the data rate on the logger was so high (240 recordings an hour), these were clearly not erroneous as they slowly crept back up to the plateau level of around 36.5°C.
I wasn't happy with this result, so I repeated it the following night. The drops in temperature were still there.
On the second night, to eliminate the possibility that these variations were due to environmental changes, my room temperature was monitored with another probe, and it was a surprisingly constant 18°C for most of the night, so there were no corresponding dips in room temperature. I don't like my bedroom to be too warm so I switch the heating off at night.
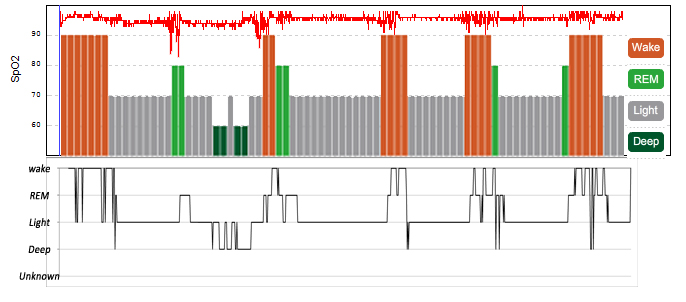
I took a look at my sleep-stage data using the Zeo, and was surprised that the seemingly random falls in temperature coincided with awakenings from REM! (Shown as orange "wake periods" on the coloured graph, but as REM/Wake on the detailed graph. Light green = REM, Dark green = slow wave sleep, grey - stage 1 & 2 sleep. For the sake of simplicity I won't show the detailed graph, but you can see one on the blog post "My Baseline AHI").

So what's going on?
Along with the muscle paralysis that comes with REM sleep (to stop us acting out our dreams), there is also a decrease in the body's ability to regulate its temperature (thermoregulation).
So, it seems that my temperature was dropping, causing me to wake in order to regulate my temperature, pretty much in the same way that my apnoeas cause me to wake during REM.
If this is true then it means that in order to be able to stay asleep during REM I now have two issues to deal with: apnoeas AND temperature!
During REM this decrease in ability to regulate our temperature causes us to be largely "Poikilothermic" (meaning that our temperature is governed by the temperature of our environment). So the key to eliminating this issue is to regulate the temperature of my bedroom better.
I repeated this for two more days, and then concentrated on the nights and gathered more data (total of 5 nights). It seems that these overnight drops in temperature aren't always correlated with REM sleep (sometimes they are just before and sometimes just after), so until my more accurate thermometer arrives, I decided to calculate the mean temperature from the week's recordings to get a better idea of my rhythm and to try to eliminate the overnight drops.

This gives a much nicer picture and goes some way to reducing the environmental effects. The data fits well with how I feel throughout the day. I tend to get a bit tired at 1pm, then start considering bed around 8-9pm.
Compared to the BBC graph, it lines up fairly well, although my "energy drop" happens earlier in the day at a more accurate time.

I'm not comfortable with this experiment as there is much that could be improved on:
- Better temperature sensor (on it's way)
- Eliminate environmental temperature effects (maybe on a day where I stay at home)
- I still am not convinced whether these changes in temperature are an effect of activity. After all, it stands to reason that when we are more active our bodies produce more heat, so it would be interesting to do this on a day where I forced myself to do nothing, stayed at home and forced myself to stay awake past my usual bedtime, that way I could see whether these changes are still evident on the graph. That said, some of the nights were recorded with an 11pm bedtime although my temperature still dropped as usual around 8pm, so it could be accurate.
One thing that it has shown me is that it is essential to have your sleeping environment just right for you...
A good sleep routine involves making sure that your bedroom is the right temperature. It should be cool but not cold. In days gone by, the outside temperature dropping in the evening acted as a cue for our ancestors' bodies to sleep. Of course, in days where our homes are heated, this confuses the body and can lead to poor sleep.
The same is true with light. Nowadays we have artificial light filling our homes and offices, and that also interferes with our sleep/wake cycle as we don't receive the nighttime cues.
So sunlight during the day and a cool, dark bedroom goes some way to remedying this.
 Hypnagogia Blog
Hypnagogia Blog
My new monitor arrived. It's able to record temperature, blood pressure, ecg trace, heart rate and oxygen saturations together.
I still saw temperature drops, and they still correlate with REM sleep.
The following screenshot (combined with the Zeo hypnogrm) shows the temperature drop along with changes in heart-rate during a REM period.

Key
Zeo hypnogram
Oxygen saturations
Pulse rate
Temperature
 Circadian,
Circadian,  REM energy,
REM energy,  Rhythm,
Rhythm,  logger,
logger,  sleep,
sleep,  temperature,
temperature,  thermometer,
thermometer,  under arm | in
under arm | in  Experiment,
Experiment,  Explanations,
Explanations,  Monitors,
Monitors,  Substances
Substances