5-HTP : Modes of Action?
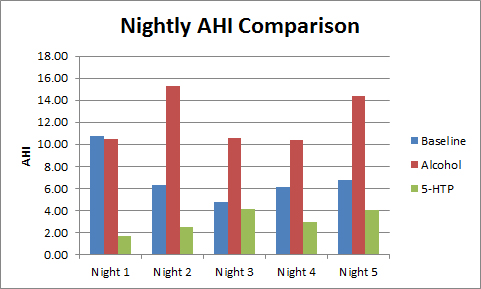
I've previously conducted two experiments with 5-HTP:
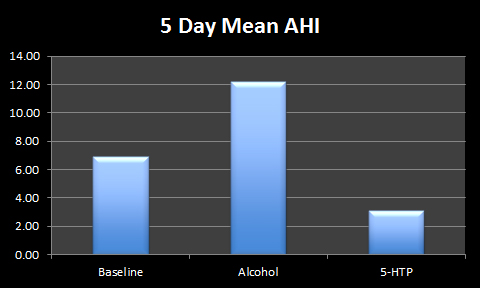
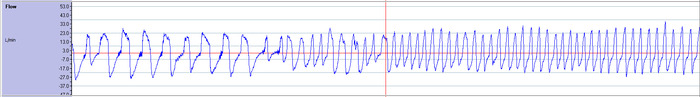
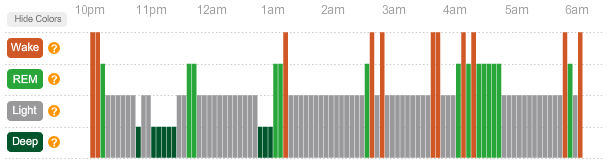
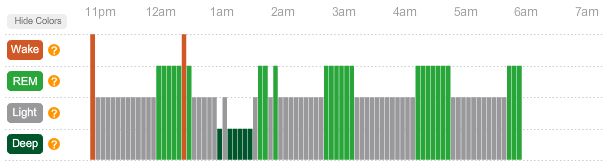
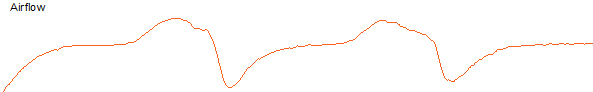
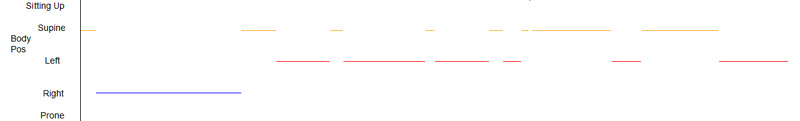
5-HTP and its effect on my AHI and sleep in general (link)
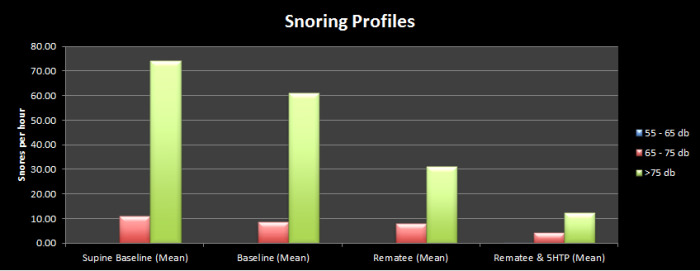
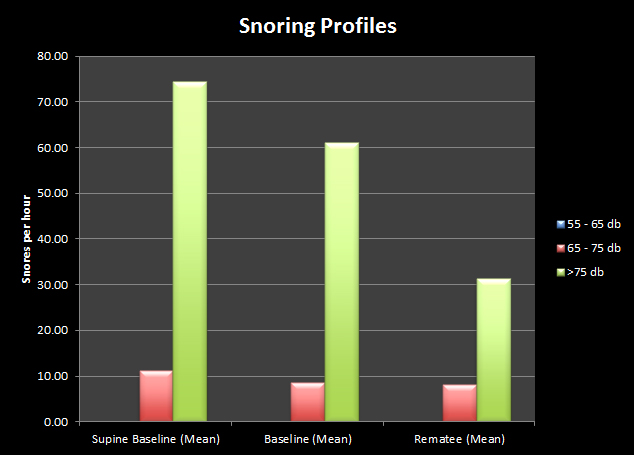
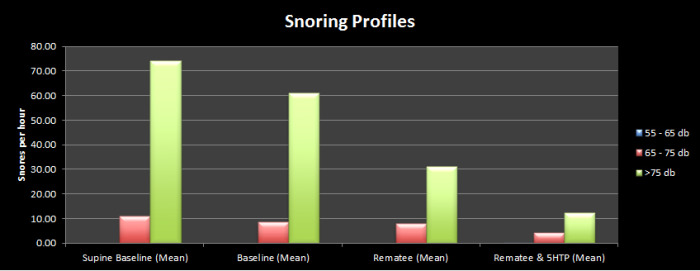
5-HTP and its effect on my snoring profile (link)
Both gave encouraging results. In fact they were so encouraging and surprising that I really would like to know more about how it has the effect that it does, and would it work for other people?
My studies are so small (as I am only experimenting on myself) and the potential for a pharmaceutical solution to Sleep Apnoea and Snoring so attractive that I would love to see further research and a larger trial for 5-HTP as it poses so many questions:
- Does it work for anyone other than me?
- Is it only effective for Mild Obstructive Sleep Apnoea?
- How dose-dependent are the effects? Does too high a dose limit the effectiveness (as with Melatonin)?
- Does the positive effect fade with long-term use?
- Are there any negative effects?
- Are the co-factors that I've been taking with this brand of 5-HTP (label from manufacturer's website here) partly responsible for the effect?
Although I can't find the results of any direct studies looking at AHI or snoring, there is a fair amount of medical literature relating to Serotonin (which 5-HTP is an immediate precursor to, that is 5-HTP is metabolised into Serotonin by the body).
From the existing literature I've tried to piece together possible mechanisms for the effects that I've observed.
THE EFFECTS OF SEROTONIN ANTAGONISTS IN AN ANIMAL MODEL OF SLEEP-DISORDERED BREATHING
By blocking serotonin activity in a breed of dog prone to obstructive apnea, it was possible to induce snoring whilst they were awake along with a collapse of the upper airway, which was reversed when serotonin activity was allowed to return.
Veasey SC, Panckeri KA, Hoffman EA, Pack AI, Hendricks JC
http://ukpmc.ac.uk/abstract/MED/8564132
"Veasey et al" blocked the action of serotonin (5-HT) in Bulldogs while they were awake (using agents known as 5-HT Antagonists). Daytime snoring was observed. Furthermore using live CT scanning a collapse of the upper airway was observed. These effects were reversed when the action of serotonin was unblocked.
This gives a clear indication that serotonin is essential for maintaining the muscle tone of the upper airway.
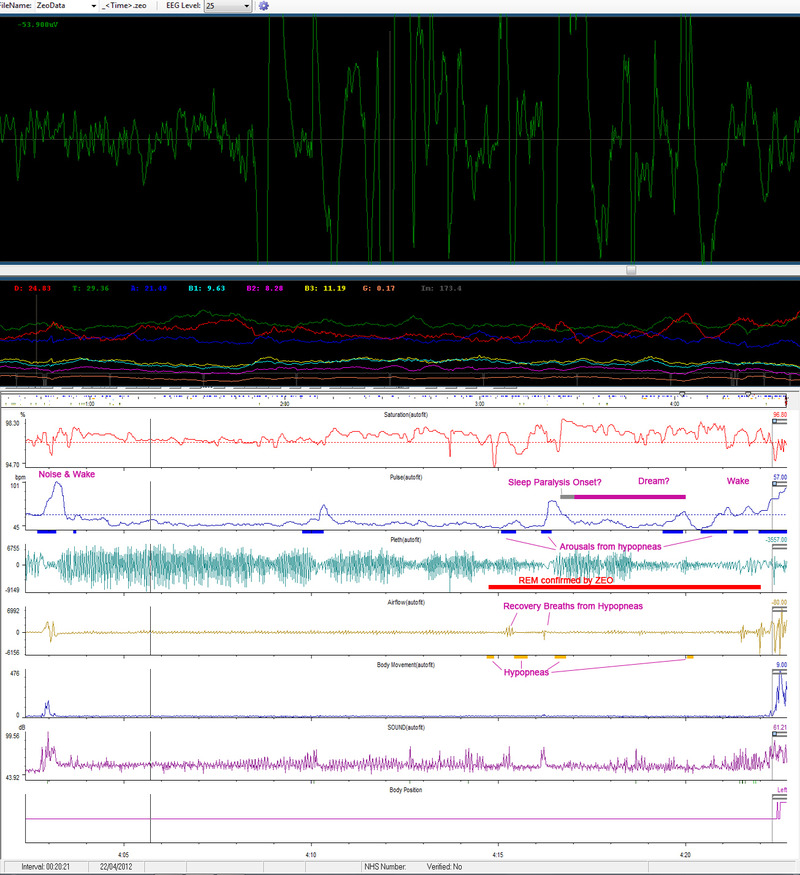
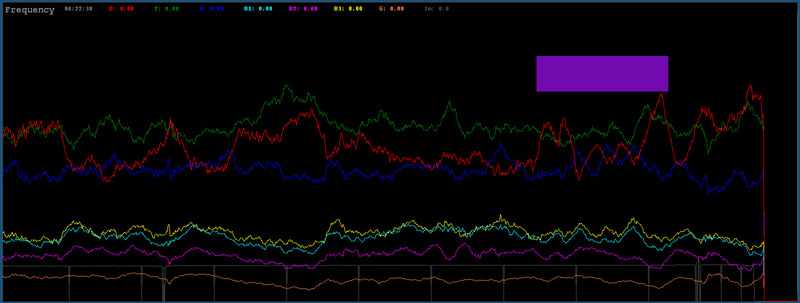
So, why does this tone drop off during sleep? During sleep (and especially during REM sleep) muscle tone is reduced. In REM sleep we undergo muscle atonia (deactivation of most muscles - this is also the cause of sleep paralysis). It is also shown that Serotonin activity is at its lowest during REM sleep. So a greatly reduced level of serotonin activity leads to a greatly reduced level of muscle activity during REM sleep.
It doesn't seem that simply activating certain Serotonin receptors can undo this muscle atonia. This is a bit of a leap on my part, but it seems that 5-HTP excites all types of serotonin receptors rather than just a few that are excited by various other pharmaceutical methods. Maybe this is because that by allowing the body to convert the extra 5-HTP to serotonin you are allowing natural metabolism of 5-HTP to 5-HT rather than just a localised or specific 5-HT receptor activity.
There are papers that support the fact that 5-HTP has an effect where 5-HT has none (albeit in motor function).
5-HT PRECURSOR LOADING, BUT NOT 5-HT RECEPTOR AGONISTS, INCREASES MOTOR FUNCTION AFTER SPINAL CORD CONTUSION IN ADULT RATS
Y. Hayashi, S. Jacob-Vadakot, E.A. Dugan, S. McBride, R. Olexa, K. Simansky, M. Murray, & J.S. Shumsky
Exp Neurol Jan 2010
We conclude that selective 5-HT or 5-HT receptor activation was not effective in improving 2C1A hindlimb function after incomplete lesions. In contrast, the 5-HT precursor 5-hydroxytryptophan (L-5-HTP), which activates all classes of 5-HT receptors, increased both %WS and hindlimb activity
http://ukpmc.ac.uk/abstract/MED/19840787
In the following paper by Ling, Bach & Mitchell it is shown that 5-HTP has the ability to reveal and activate a latent pathway in the spinal cord in hemisected rats (similating an incomplete spinal injury).
SEROTONIN REVEALS INEFFECTIVE SPINAL PATHWAYS TO CONTRALATERAL PHRENIC MOTONEURONS IN SPINALLY HEMISECTED RAT
Liming Ling, Karen B. Bach, Gordon S. Mitchell
Exp Brain (June 1994)
These results indicate that serotonin converts ineffective crossed phrenic pathways in the spinal cord to effective pathways. It remains to be determined whether serotonin is both necessary and sufficient in this modulatory process, or if it is a nonspecific result of increased phrenic motoneuron excitability.
http://ukpmc.ac.uk/abstract/MED/7843300
5-HYDROXYTRYPTOPHAN-INDUCED RESPIRATORY RECOVERY AFTER CERVICAL SPINAL CORD HEMISECTION IN RATS
Shi-Yi Zhou & Harry G. Goshgarian
J. Applied Physiol (June 2000)
Because experiments were conducted on animals subjected to C2 spinal cord hemisection, the recovery was most likely mediated by the activation of a latent respiratory pathway spared by the spinal cord injury. The results suggest that serotonin is an important neuromodulator in the unmasking of the latent respiratory pathway after spinal cord injury.
http://ukpmc.ac.uk/abstract/MED/11007592
So we have two potential mechanisms by which 5-HTP could work:
- By loading with 5-HTP it allows the body to metabolise it to 5-HT activating all classes of 5-HT receptors thereby reducing the effects of muscle atonia in REM without completely inhibiting REM atonia.
- By possibly activating a dormant pathway in the spine to the phrenic nerve (increasing breathing effort).
As we've seen by my sleep-study results, my sleep apnoea is obstructive in nature, so it is unlikely that increasing breathing effort would reduce my AHI as I still make breathing movements but they are rendered ineffective by the obstruction in my upper airway.
If 5-HTP does work in these two ways then it's possible that 5-HTP may have a positive effect on both Obstructive and Central sleep apnoea as item 1 above relates to OSA while item 2 relates to some forms of CSA.
 5-HTP,
5-HTP,  Literature Review | in
Literature Review | in  Discussion,
Discussion,  Explanations
Explanations