CPAP - It's well worth taking the time to get it right
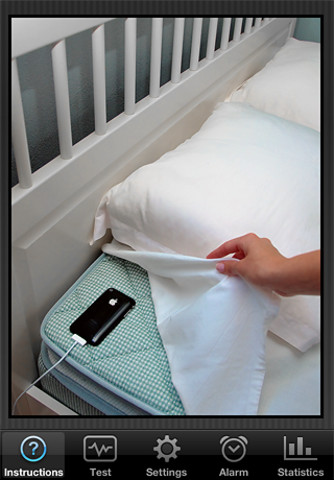
Previously I'd used CPAP for a few days to try to get an idea of how my son felt as he started to use it.
Initially I tried it in the hospital where it was prescribed. I used it whilst awake using a variety of masks and pressures to see what high pressures felt like and to see how it responded to me exhaling, holding my breath, trying to talk and opening my mouth etc. Then I used it for a few nights. I wanted to know what problems he could encounter because he isn't able to move to correct them for himself, so I thought that if I were familiar with some of the problems it'd at the very least give me a frame of reference for when he told me what issues he was having.
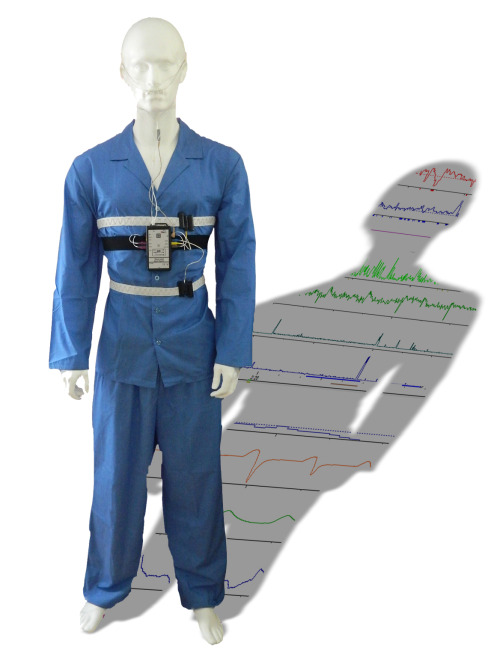
For practical reasons I purchased an additional CPAP (technically an APAP machine - Auto CPAP). I chose the Resmed S9 Autoset, which to its credit doesn't look like a piece of medical kit; it looks more like a modern bedside clock radio. Yes, the pressures should be set by a professional and you need a prescription to buy one but it looks like a piece of consumer electronics, which is a great thing because it doesn't make your bedroom look like a High Dependency Unit.
Resmed also make coloured "skins" for the device which would be helpful when trying to introduce it to children as part of their therapy.
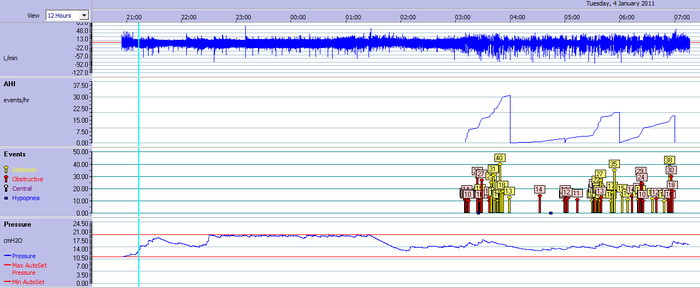
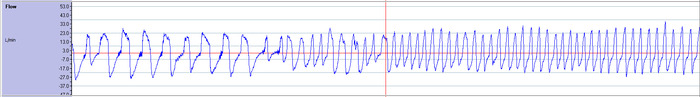
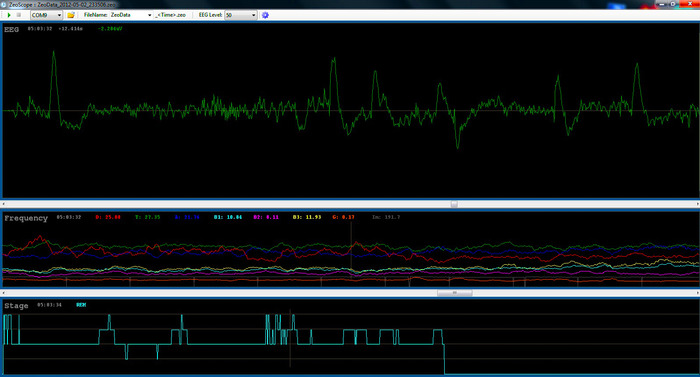
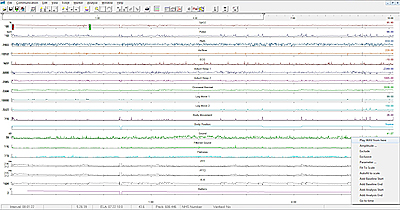
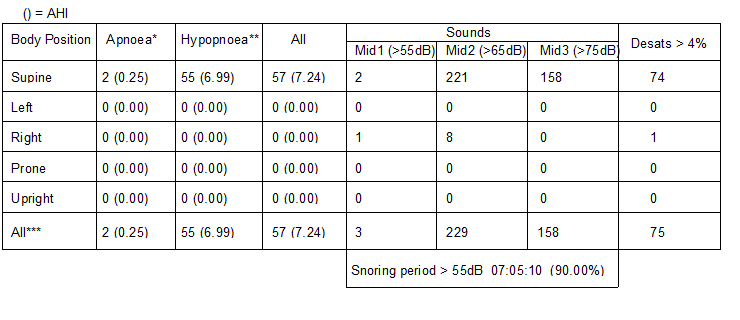
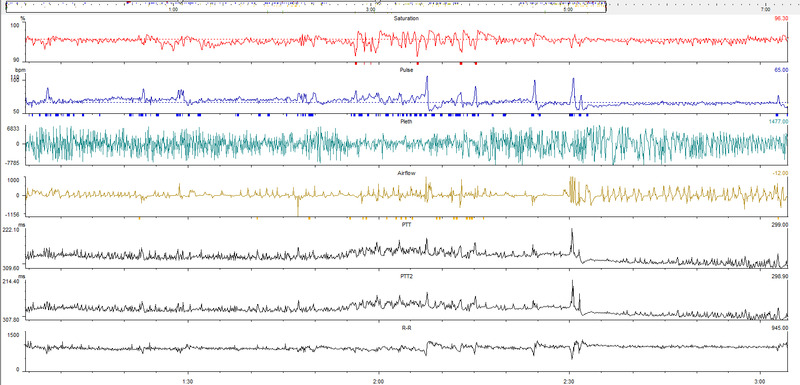
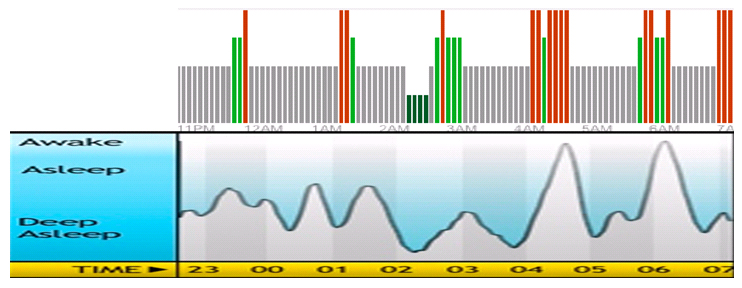
The S9 records overnight summary data and detailed data to an SD card, which via the ResScan software allows you to see the following data:
- Respiratory Events via flags on the timeline (Central Apnoeas, Obstructive Apnoeas and Hypopneas)
- Pressures chosen by the machine at any given time
- An indication of snoring level
- Flow (allowing individual breathing waveforms to be seen)
- Leak
- Flow Limitation (an indicator of the degree of obstruction)
- Compliance data (how long I used it for)
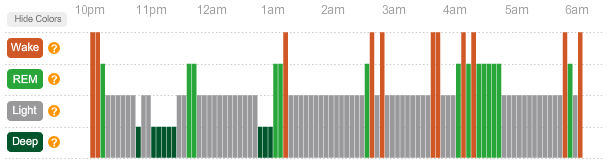
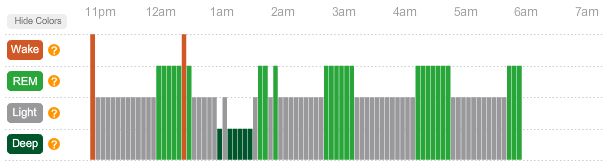
An example of the data from one of the nights that my son used it is shown below.
All of this is very useful to have access to because it lets you see a record of the choices that the machine makes which helped me to trust that the machine wasn't going to deliver a high pressure unless there was a good reason to. This is all recorded automatically while you sleep at home (or in the sleep lab). Compared to a one-night study in a sleep lab (especially a split night study) the data may be a more realistic representation of your sleep because you'll be sleeping in a familiar place and adhering to your usual routine.
The output that we collected from the ResScan software was viewed by my son's doctors during his initial trials with CPAP before changing over to Bi Level ventilation (BiPAP / VPAP / BPAP)

I chose Resmed's Swift FX Nasal pillows as they left a lot of my face free, they didn't feel trapping and are easy to remove if I really felt like it in the night.
My son uses them with Bi-Level PAP and prefers them over a wide range of masks that he's experimented with, although he can't move below his shoulders he has learned to remove the Swift FX pillows by a head movement, so he feels comfortable using them as he knows that he can take it off if needed.
The S9 has an "AutoSet" mode where it can alter the delivery pressures as it deems necessary. The machine can be forced to work within a range of pressures. I decided to let the machine have a free reign and didn't force it to choose between limits.
I managed to keep the CPAP on for most of the night, but I remember waking frequently and moving the tubing and to keep checking the machine because... well to be honest... I was nervous. The machine is very quiet which was another reason to check it every time I stirred in the night in case I'd managed to turn it off in the same way that I snooze the alarm clock.
Over the few days I was tired because, as I said above, I'd been awake due to my own anxiety and the strangeness of it all, also I managed to get caught up in the tubing one night! The following evening I arrived home from work and dived face down into bed without CPAP. Due to my sleep debt over the previous few nights I experienced sleep paralysis and a lucid dream, so it wasn't all bad.
...and that's where my trial with CPAP ended.
However, recently I've fallen in love with CPAP and in particular Resmed's S9 Autoset (the photo above is my S9 beside my bed), and here's how it happened...
There's a lot to get used to with strange tubes and masks on you and your bed plus a new machine on the bedside table - and that's without getting used to the pressures that the machine delivers... considering this, my experience wasn't really a fair trial for CPAP, especially since it is considered to be the "Gold Standard" in treating obstrucitve sleep apnoea.
In hindsight, I suspect it would have been better to begin by choosing a low pressure and just wearing it to get used to the mask and tubing - almost a dress rehearsal before the therapeutic pressures are used.
My CPAP experience was well over a year ago and before the time that I started this blog and before the time that I realised that I had mild to moderate obstructive sleep apnoea. Now that I have a better understanding of my own sleep and have found various ways to reduce my AHI without CPAP I decided to give it another go and compare the results, after all we now had my son's "old" (barely used) S9 Autoset sitting in a cupboard doing nothing because he actually needed Bi-Level PAP.
This time I paid a lot more attention to my own AHI.
I also decided to eliminate the uncertainty of whether the machine was going to wake me with a high pressure during the night, so I did a gradual titration over several nights using the "Straight CPAP" setting of my son's backup Respironics BiPAP S/T.
I found myself making slow deliberate breaths while I tried to sleep. This wasn't particularly helpful, because (even if you aren't wearing CPAP) when you think about your breathing you find yourself consciously taking over, and to be honest this is something that our bodies do better if we don't let consciousness interfere with it.
However, I found myself calmly waking up every now then wondering why I wasn't breathing and finding that I had to consciously take a breath, I listened to machine respond, then dropped back off to sleep. This happened maybe 5 or 6 times that I remember during the night and wasn't anything like waking with a snort or a choke, in fact it felt quite strange.
In the mornings I took a look at the data (the BiPAP S/T also records data to an SD Card that is readable via the Respironics Encore Viewer or Encore Pro software.
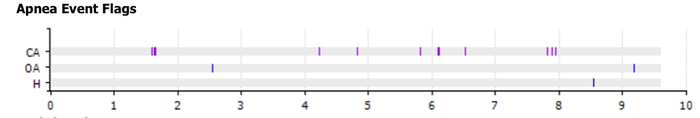
I found an explanation for the breathless awakenings...
Whilst the obstructive apnoeas were few and far between, the machine had detected "Central Apnoeas". These are when the airway is open yet no air flows. This can be from a variety of causes, but from my own baseline sleep studies I know that my apnoeas are usually obstructive in nature, so I knew that these new Central Apnoeas were because my chosen pressure was too high.
If breathing is too effective at clearing CO2 from the bloodstream then central apnoeas can occur because during normal breathing the brain sends a signal to breathe when CO2 in the bloodstream reaches a certain trigger level. We then breathe causing gas exchange, (taking oxygen in and exhaling CO2), after which our bodies produce more CO2 which reaches the trigger level and the cycle begins again.
If the CO2 level is too low then the brain doesn't need to clear it, so doesn't send a signal to breathe. Our oxygen levels then drop which wakes us up and allows us to consciously take a breath.
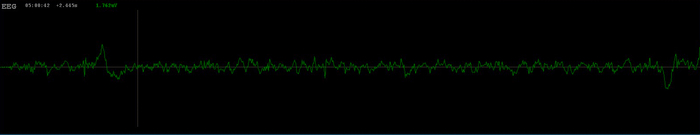
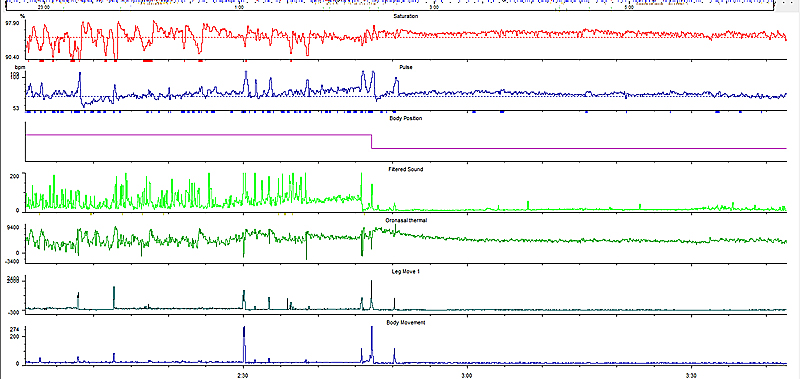
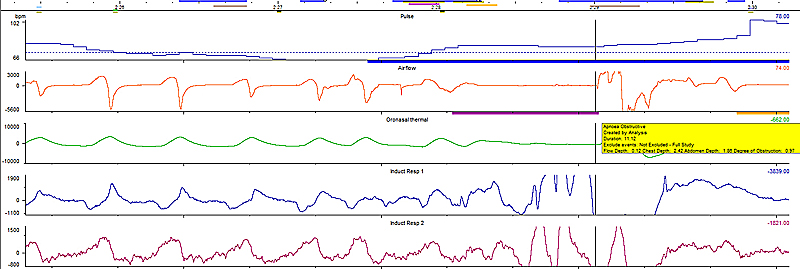
I adjusted the pressure down by 1 cmH2O the following night, but I still wanted more data. Were these really "centrals"? A night wearing the Black Shadow Sleep Monitor whilst on CPAP confirmed that they were.
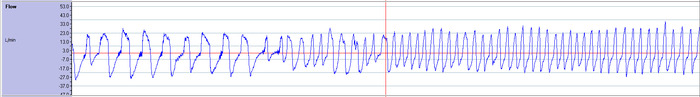
I switched machines back to the Resmed S9 Autoset because it allows you to see a lot more data as opposed to the trend data given by the Respironics BiPAP S/T. It actually allows you to look at the data at a much higher resolution (you can see every breath taken) so I could then verify any detected apnoeas for myself.
Along with the lower pressure setting, I set the S9's EPR (Expiratory Pressure Relief) to full (3) which drops the pressure down by 3cmH2O (or 1 or 2 cmH2O, depending on your chosen setting) when it detects that you are exhaling. This is very helpful, even for psychological reasons as not only does it help you to exhale, but it provides a form of tactile feedback letting you know that the machine is "listening" to you and not trying to force a gale into your nostrils whether you like it or not.
One interesting thing that the S9's additional data allowed me to see was the moment that I stopped doing those forced breaths I that I mentioned above. This is the moment that I fell asleep.
I fell asleep fairly quickly, and woke once when I turned onto my side and found that I needed to adjust the nasal-pillows slightly.
The following morning I checked the data and found that the central apnoeas had cleared and my AHI was a very respectable 0.4 which varied over the next few nights but still remained under 1.0.
One night I found that the S9 data showed that I'd been quietly snoring, it was also on this night that my AHI was the highest that I've had so far whilst on CPAP (0.9), although this is still a fantastically low AHI.
So the next night I crept the pressures up by 0.4 cmH2O, only to find that the snoring cleared but some central apnoeas returned, so I dropped the pressures again. It became obvious that finding a pressure that was perfect for every night was going to be a challenge.
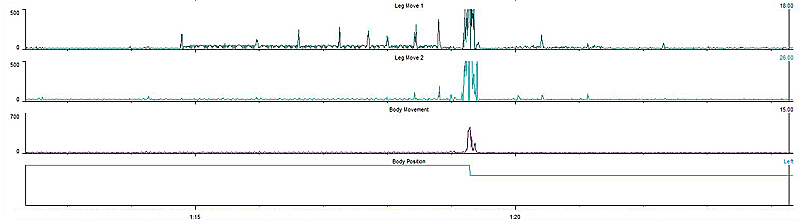
Of course I realise that there is going to be some "natural variation" from night to night due to factors such as body position and time spent in each sleep stage but wouldn't it be good to be able to pin down what the other less obvious variables are?
My main factors are related to body position (apnoeas are more likely and frequent when I sleep supine) and REM sleep (when muscle tone is decreased in the airway), but I suspect that other factors during the day play a part.
This is where the S9 Autoset excels: In AutoSet mode it adjusts the pressure it delivers based on your need at the time, so where "Straight CPAP" is limited because it can only give me one pressure throughout the night meaning that 8cmH20 may be too much for me at some parts of the night (causing Central Apnoeas), yet not adequate for other parts of the night) where 10 or 11 cmH2O is more appropriate.
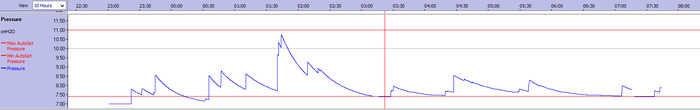
I set my S9 to "Autoset" mode and adjusted the settings so that the machine would work within fairly restrictive limits just to get me comfortable with the idea. In the morning I could see from the ResScan software that the machine had delivered the maximum permitted pressure at some points in the night, so I gradually extended the pressure range over a few nights until the machine didn't reach my ceiling limit and was able to deliver the necessary pressures.
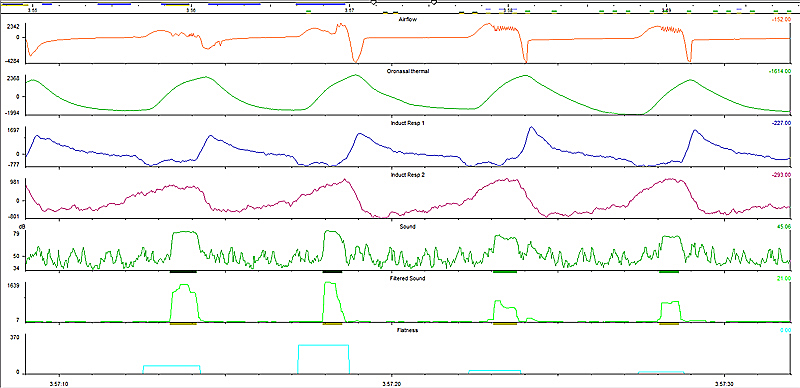
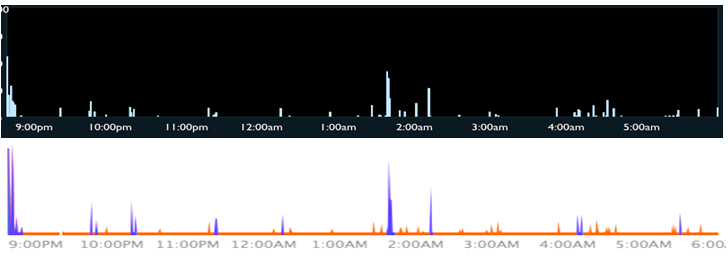
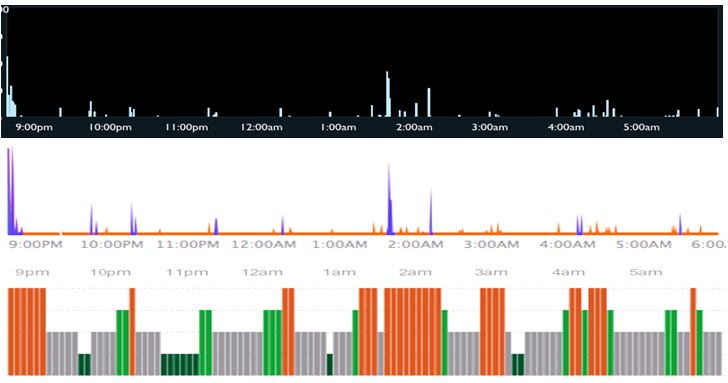
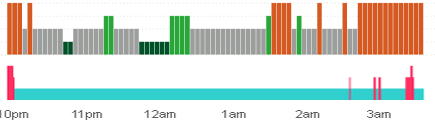
The following graph of the pressure that the S9 delivered over one of the later nights illustrates how my requirement varies through the night.
On the night above I woke myself up snoring after several hours (just before the red vertical line), so I raised the lower limit and went back to sleep, this is why the graph above shows the delivery of pressure that is lower than permitted minimum pressure at the start of the night.
Had I been prescribed straight CPAP based on the pressures titrated on this night then I would have had to have a constant pressure of between 10 and 11 cmH2O to eliminate all my obstructive apnoeas. However, the chances are that I would have then had more central apnoeas occurring. A compromise pressure of 9 cmH2O would have removed the majority of apnoeas but would have been inadequate when my obstructions were at their most severe. There could also have been central apnoeas occuring at this pressure for some of the night.
The textbook, "Sleep Medicine Pearls" by Richard Berry MD describes this well with a case study of a patient unable to tolerate the high pressures needed to treat his obstructive apnoea. If you have access to the book you can find the details under Patient #43. In fact the whole book is packed with case studies that provide a unique insight into treating sleep issues.
If high pressures can't be tolerated it may be preferable to have a lower than optimal pressure setting just to ensure that some benefit is obtained, although it is likely that these patients would benefit more from Bi-Level PAP which allows a much lower expiratory pressure.
In Autoset mode, the S9 allows low pressures but can deliver the higher pressures when necessary, giving you the flexibility (and comfort) of both in one setting.
Some good news: my nose isn't as big as I thought...
I found that I woke up several times in the night and had to adjust the nasal pillows but each pack of Swift FX nasal pillows come with three sizes of pillows. I found that when I decreased the size of the nasal pillows to the medium size (although the large were comfortable and the leak minimal) the medium pillows were more comfortable and needed a lot less adjusting when I first put them on and hardly any throughout the night.
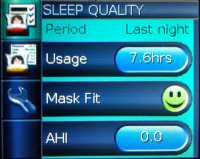
I slept really well and took a look at the display screen on the S9 when I woke.
I was greeted by an AHI of 0.0 and a green smiling face telling me that the nasal pillows were a good fit and weren't excessively leaking.
The ResScan software also confirmed the Zero AHI.
Now that I use the Autoset mode, my AHI is always under 1.0 regardless of what position I sleep in or even if I've had a glass of wine.
It actually feels good to sleep on my back again, I'd been using the Rematee side-sleeping belt for a while and found that I missed sleeping on my back. With CPAP I didn't ache when I woke up. CPAP was surprisingly unrestrictive and I soon learned a manoeuvre to clutch the hose and move it with me if I wanted to turn in the night.
To be fair I could have just let the S9 go on full unrestricted auto from day one and it would have delivered the same pressures, but from mine and my son's previous experience with Non-invasive Ventilation, a large factor in whether it is successful is down to whether the sleeper (patient) feels comfortable with it, yes the numbers are important (after all that is the whole point of the therapy), but the patient experience is also key as that alone will probably be the biggest factor in whether they are "compliant" with it (ie use it for 4 hours or more a night), after all many PAP machines don't allow the user to see their AHI data so they can only judge based on how it feels.
Another part of the experience is the mask that is used. There is a wide choice of masks available, and it's important to find one that is right. Also humidification can help people feel more comfortable with PAP therapy, this is something else that should be available to them along with all manner of accesories such as hose holders - really anything that will prevent someone giving up. That said, CPAP therapy isn't right for everyone as my son's situation shows, so good communication with a committed Sleep Consultant is vital in order that the right treatment be offered.
I think looking into things in this detail was necessary for me, although it was a rather involved way of getting used to CPAP and trusting it, it has been well worth it. I feel a lot more awake in the mornings (generally only sleeping for 7.5 hours now) and my AHI has been consistency the lowest it has been in probably 20 years.
I think the graph below speaks for itself.
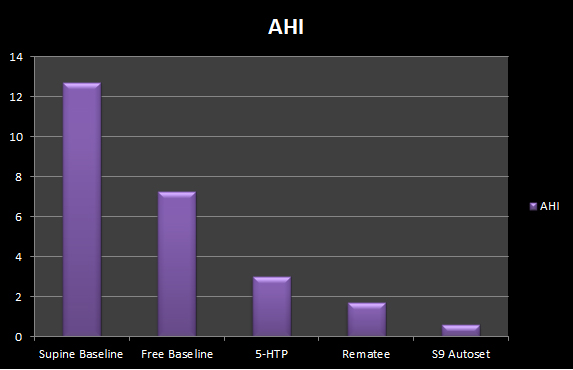
CPAP is a clear winner and one that is likely going to be impossible to beat but that's not going to stop me trying out other apnoea remedies to see if they can come close.
CPAP has also made a huge difference to my snoring, the results of which I'll post in a few days.
For the future:
- I'd like to see if the pressure requirement decreases if I take a dose of 5-HTP at bedtime.
- Although I don't intend to change my nasal pillows, I would like to see what difference other masks make to the experience.
Useful Links
Michael F. Fitzpatrick, Christi E. D. Alloway, Tracy M. Wakeford, Alistair W. MacLean, Peter W. Munt and Andrew G. Day
Can Patients with Obstructive Sleep Apnea Titrate Their Own Continuous Positive Airway Pressure?
(full text PDF available to non-subscribers via the link)
Gao W, Jin Y, Wang Y, Sun M, Chen B, Zhou N, Deng Y.
Is automatic CPAP titration as effective as manual CPAP titration in OSAHS patients? A meta-analysis.
 APAP,
APAP,  CPAP,
CPAP,  Home,
Home,  Nasal Pillows,
Nasal Pillows,  Non invasive ventilation,
Non invasive ventilation,  ResMed,
ResMed,  Respironics,
Respironics,  S9 AutoSet,
S9 AutoSet,  Swift FX,
Swift FX,  Titration,
Titration,  xPAP CPAP Richard Berry | in
xPAP CPAP Richard Berry | in  Apnoea,
Apnoea,  Experiment,
Experiment,  Monitors,
Monitors,  NIV
NIV