Sleeping Position: Get off your back!
When you have a multi-channel sleep study, one of the "channels" that is examined is the position that you sleep in.
At first this may seem a strange thing to monitor, after all if you manage to achieve sleep, who cares how your inert body is positioned?
Sleep position affects several aspects of our sleep, for example when I sleep on my back I find that:
- I experience more sleep paralysis
- I experience more body twitches as sleep begins
- It's also known that breathing is harder when sleeping flat on your back (supine), it is for this reason that patients with higher level spinal injuries are recommended to sleep with their head inclined and foot of their bed lowered as this can actually increase their vital capacity
- GERD / Acid Reflux / Heartburn is affected by sleeping position. Raising the head of your bed can prevent or at least reduce reflux episodes.
However, in this blog-post I'm going to concentrate on another major effect that supine sleeping has on the sleeper...
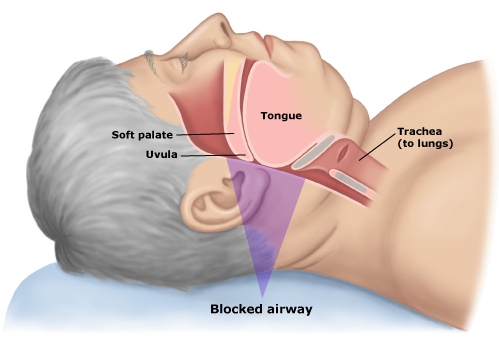
Supine sleeping can dramatically increase the number of obstructive apnoeas and hypopneas a sleeper has through the night!
The reason for this is that gravity has a greater effect on the muscles and soft tissues that relax in sleep and cause obstructive apnoeas. If you can lie on your side then gravity doesn't affect them in the same way, and can go some way to keeping the airways open during sleep.
Invariably we move around in our sleep so I needed a way to monitor my sleeping position as my monitor doesn't have this ability.
More sophisticated sleep study devices do this automatically, and there is actually an iPhone app that can do this for you too: Somnopose, after a couple of night of experimenting with the app you should be able to get a fairly accurate reading. You will probably be surprised how many times you actually turn over in your sleep.
This was actually quite easy for me to do manually as I already had my infra-red camera watching me for several nights during sleep. I then analysed the video to determine my sleep position. As well as recording continuously, the camera creates a new file every time it detects movement, so all I had to do was flick through the files and record the position on a chart alongside my oxygen desaturations. I did also plot a chart of body position against detected apnoeas, but the chart below shows things clearly enough.
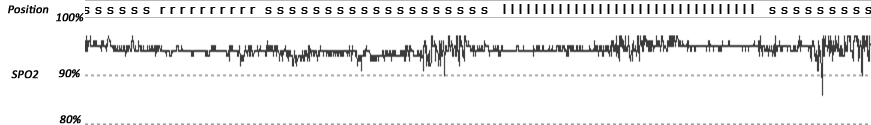
s=supine (back), p=prone (front), l=left down, r=right down
It was no surprise to see that the majority of my apnoeas and hypopneas occurred when I was sleeping on my back.
On several nights I deliberately began sleep on my side, but always woke to find myself flat on my back again and with a high AHI recorded. I needed a way to prevent myself from turning over in the night.
Years ago, a solution to positional obstructive sleep apnoea was to "sew a tennis ball into the back of your pyjamas", this had a "Princess and the Pea" type effect on the sleeper and caused them to be uncomfortable if they turned over and slept on their back.
Nowadays there are more sophisticated solutions, and the one that I put to the test is called the "REMATEE Bumper Belt". It's a neoprene belt that velcro fastens around your chest. At the back of the belt are pockets into which you place inflatable "bumpers". Sounds strange?
It may be clearer if I show you a photo of what I'm describing. Rather then subjecting you to a screen-capture from my camera, I'll use a product photo instead (click for a larger version).
It's surprising how quickly you get used to it.
My belt also has shoulder straps to stop it turning round in the night although when it first arrived I was slightly daunted by the idea of being strapped in, so I decided to tuck the shoulder straps into the pouches that held the bumpers.
I found that if the belt was tight enough then I didn't need to use the shoulder straps, but it does take a few nights of trial and error to get used to how tight to wear it and how much air to put in the bumpers.
When the belt first arrived I tried it out for a few nights without monitoring my breathing and found that it did affect my Zeo stats. It increased my REM sleep. It also reduced the number of awakenings that I had through the night.
Initially, it seemed to decrease Deep (SWS) Sleep but this stopped and my SWS actually increased after a few nights of using it. (See graphs below).
Then I began my five nights of recording my breathing...
Again I followed my rules for determining my 5-night mean data with the obvious exception of not beginning the night by sleeping on my back. I also didn't take any of the supplements discussed in this blog, and I stopped the vitamins and minerals on the Friday beforehand to try to eliminate the effects of those on my sleep.
The results were clear:
The REMATEE belt kept me off my back and reduced my oxygen desaturations:
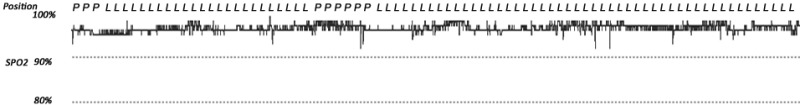
s=supine (back), p=prone (front), l=left down, r=right down
My AHI each night was dramatically reduced:
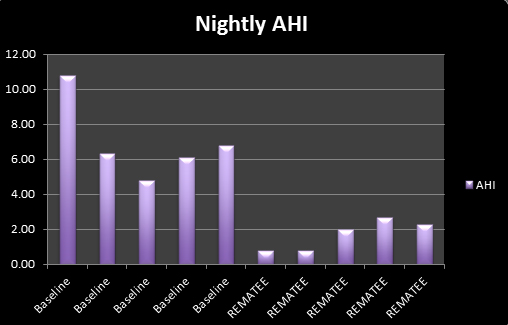
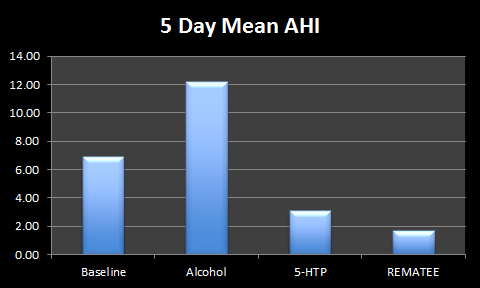
This brought my 5-day mean AHI down to 1.70.
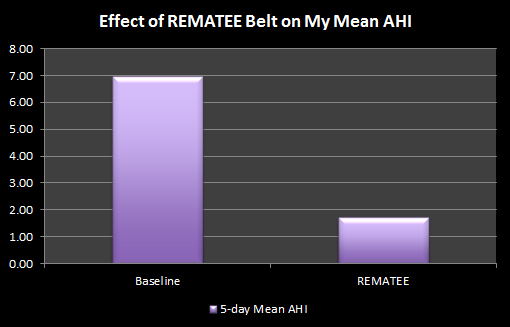
This makes the REMATEE the most effective method that I've found so far to reduce my AHI.
The reduction in respiratory events (reflected by the reduced AHI) also had a positive knock-on effect on my Zeo data...
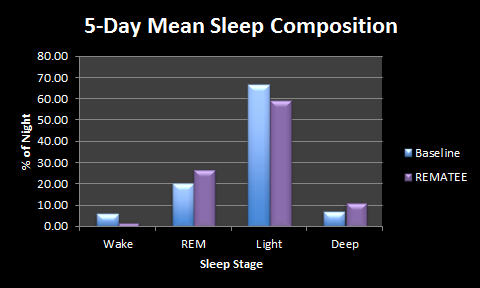
Considering that most of my respiratory events happen in REM sleep, it makes sense that when the number of events was reduced, my REM increased (because it was not being broken by me waking up to breathe). As already discussed, my Slow Wave Sleep (deep) also increased.
Will I carry on using the REMATEE? Definitely.
As a follow up, I plan to combine the REMATEE belt with my 5-HTP routine as both seem to reduce my AHI through different mechanisms. Maybe their combined effect will be greater than as individual methods.
Additional Links
The REMATEE Bumper Belt is available in the UK from Intus Healthcare:
http://www.eu-pap.co.uk/rematee-neoprene-bumper-belt.html
REMATEE http://www.antisnoreshirt.com/
 Belt,
Belt,  Bumper Belt,
Bumper Belt,  Gravity,
Gravity,  Positional Therapy,
Positional Therapy,  REMATEE,
REMATEE,  Side sleeping,
Side sleeping,  Supine,
Supine,  apnoea,
apnoea,  obstructive | in
obstructive | in  Apnoea,
Apnoea,  Experiment
Experiment