Wild Camping with CPAP
Wild Camping (also known as Dry Camping) is where you camp with a minimum of kit using what you can find around you: drinking stream water, eating plants, hunting, trapping and building shelters (think "Ray Mears" and you'll get the picture - living with nature), and it's something that I'm taking an interest in, so much so that I decided to spend a few nights "under the stars", of course my CPAP machine came with me...
Why did I decide to do to do this?
Well, after an overnight power cut at home I realised how dependent we were on technology and electricity for pretty much everything we do, and that made me feel pretty helpless, it's all very well having the kit to treat my sleep apnoea but it becomes useless without electricity. My computers became black mirrors, my freezer became a box full of water, the hot water wasn't hot... anyway you get the picture.
It's all well and good having spare masks and tubing for your CPAP, but it's another to not have any electricity!
Fortunately during the power cut we had a car jump-start battery pack to power my son's BiPAP, but at his prescribed pressures it only lasts little more than a night. I began wondering how we'd cope with more than a day without electricity.
Yes, I could charge the battery from the car and risk it flattening my car battery, or I could let him sleep in the car while I drove us to a relative's house that had electricity, but that didn't seem to be a complete solution.
Although it's unlikely that we'd be without power for more than a day, it's better to be safe than sorry. How much easier is it to change over to battery backup than to go on a midnight quest for electricity?
This made me wonder how I would cope with a minimum of kit in the wilderness. I'd camped before, even in a desert in the Middle East, but that was with a 4x4 crammed full of kit and I wasn't a CPAP user then, travelling light was the plan for this trip, and the CPAP and Jump-Start battery pack were going to be an awful lot of kit to drag along.
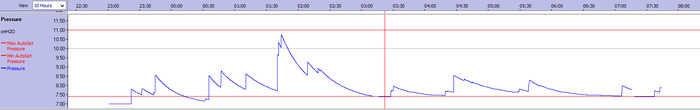
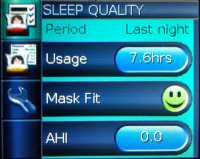
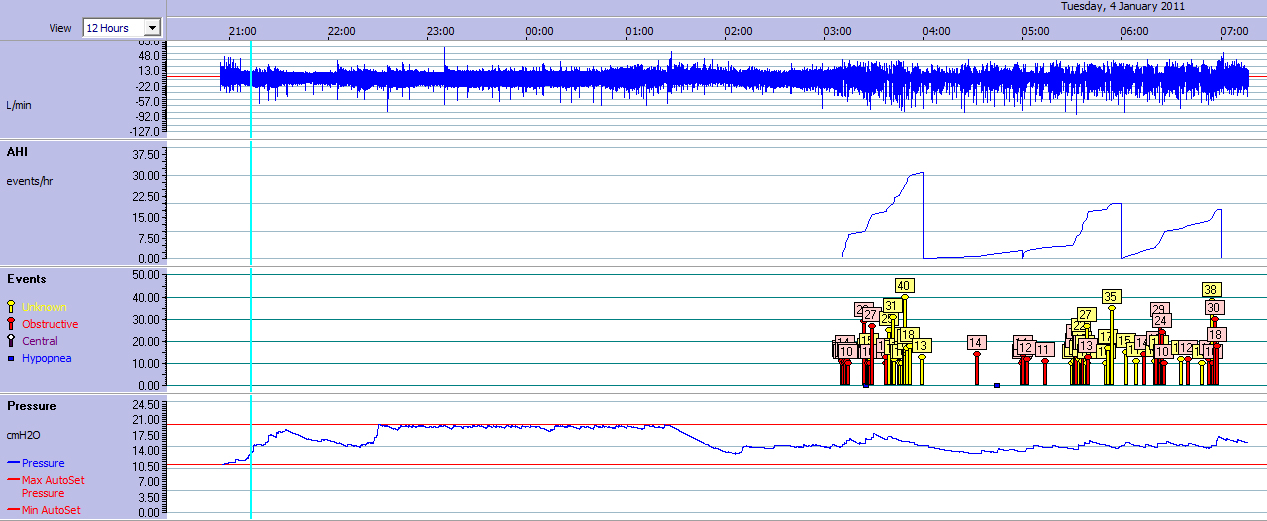
So I invested in a relatively lightweight dedicated battery and tested how long it would support my pressures at home.
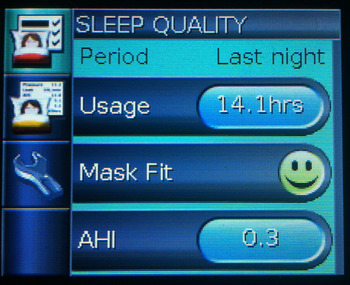
The "Super CPAP Battery" sustained my Resmed S9 Autoset machine for at least 5 full nights, so I knew it would last for my short one night stay in a woodland in Wales.
The idea of Wild Camping is that you take a minimum of kit with you, and it felt like cheating to be taking something as high-tech as my CPAP along but to be honest, I really don't like being without it now, so I decided that it was coming along. It would be my Desert Island Discs Luxury Item.
To try to cure that cheating feeling I decided that if I could charge my battery before I left using Solar energy then I was still qualified to play the self-sufficiency game without cheating.
Charging either of the batteries using Solar Power was simple and relatively cheap. I used a 13W solar briefcase from Maplin Electronics.
Camping aside, being able to do this gave me a sense of security, especially considering that if we were without power for more than one night I'd need a way to charge my son's BiPAP battery pack at home.
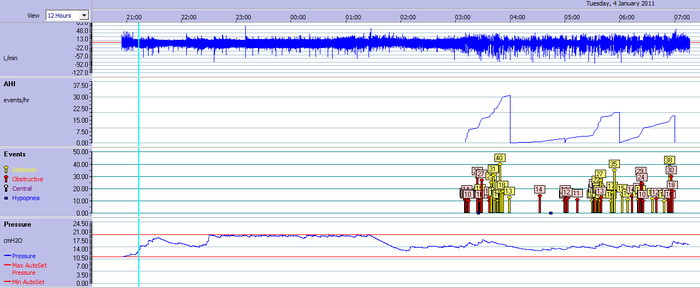
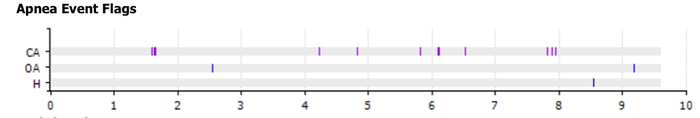
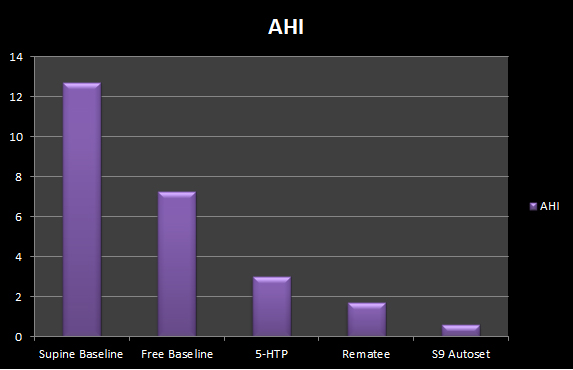
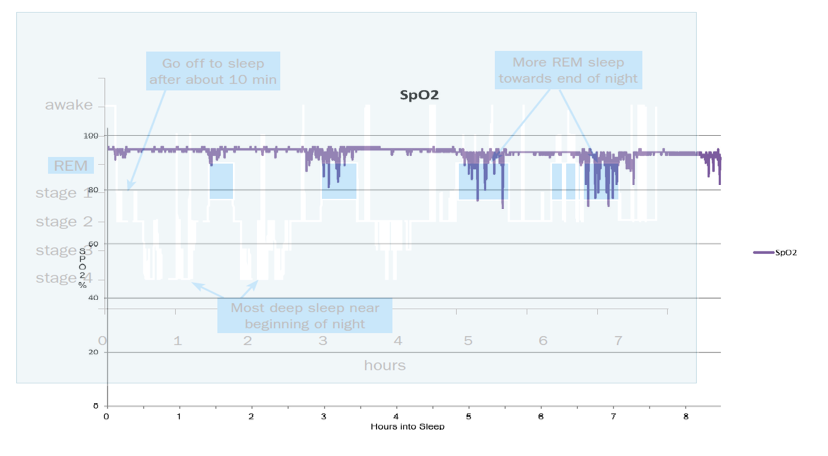
Of course I had other options, rather than taking the CPAP along for me. I could have slept on my side, but I wasn't keen on that as I often wake up uncomfortable in the mornings after using a side-sleeping device and I wasn't sure how well that would work if I ended up sleeping in a hammock. I could have taken 5-HTP but to be honest, I liked the idea of making a campfire and sharing a couple of whiskies around it with my brother, so that would likely negate the positive effect of the 5-HTP, besides, I know that alcohol has a detrimental effect on nightly AHI and hence I'd need CPAP more than ever if I drank.
I also wasn't keen on taking my shiny S9 Autoset into the woods for a night. I did contemplate buying a cheaper APAP to travel with but unless I did so and used it at home for a while I wouldn't trust the machine to behave in the same way as the S9 Autoset.
Maybe that is something that I'll do if camping becomes a regular thing for me.
After putting a few more bits of kit into my rucksack we headed for Wales with the "Super CPAP Battery" charged full of English sunshine (yes, we have some every now and then). The sunlight had travelled 96 million miles, I'm sure it wouldn't mind another couple of hundred.
This is probably the point to confess that I packed too much kit. In hindsight there is much that I would leave behind as I didn't use it, and some things that I should have taken that I didn't (a sleeping bag being the major thing that I was pining for in the night).
One of the items that I took but didn't use (although I would have done had our stay been longer) was a fantastic piece of kit called Powerfilm. This is a flexible solar panel.
The panels come in many sizes and power ratings depending on how much electricity you need. Mine was the R-15 1200 which has an output of 15.4V and is rated at 1.2A 20W. This is more than enough to recharge the CPAP battery pack even in fairly overcast conditions...
On arriving in Wales our first port of call was a shop where we were able to buy some, eggs, whisky and gloves as the weather was already worse than the forecast had indicated. Oddly this made me remember a lucid dream that I'd had about being in Wales and left me wondering what the next night would have in store for me.
We set up our camp in drizzle, so I made a simple shelter with an inbuilt groundsheet that would keep me and my kit dry.
In hindsight I should have sheltered in it until the drizzle stopped and then built something that offered more protection from the cold.
We took the Sawyer Point Zero Two water purifier with us, this filters everything out of the water that is larger than 0.02 microns. That means that all bacteria and viruses were removed. I suppose that you could use this to provide water for a humidifier, but I am so used to boiling water at home for when I used a humidifier that I'd still boil it anyway, not least because it would help with preventing limescale buildup in the humidifier tray.
Once the filter was hung from a tree we built a fire and I unpacked my CPAP setup ready for the night.
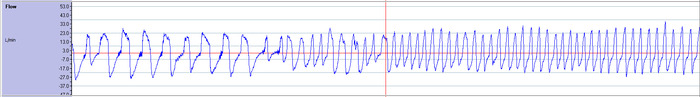
Fortunately the CPAP battery was more reliable than our fire (which lasted about 3 hours into the nighttime rain). The CPAP battery lasted all night despite it being cold (which I feared would affect it).
After a cold night I woke to find that everything (including me, the battery pack and CPAP) was covered in a heavy layer of dew and a touch of frost but it was still working.
The other thing that I noticed was that a great deal of my kit had been slimed by a slug or a snail!
This night proved to be a good test of the kit that I'd taken but it also showed me where I was going wrong. I can assure you that the massively lower than predicted 4ºC felt awful during the night without a sleeping bag!
For the following night we headed a couple of hundred miles south-east to Stonehenge for a night of hotel survival.
On arrival at the hotel, after foraging for the room service menu and having a nice hot shower, I realised that I wasn't prepared for the night because I didn't have the mains power lead or an extension lead with me to power the CPAP but fortunately the battery pack had more than enough power to last the night, and it meant that it could sit on the bedside table under the S9 leaving the room cable-free.
So while the power-pack discharged its battery I was able to recharge mine...
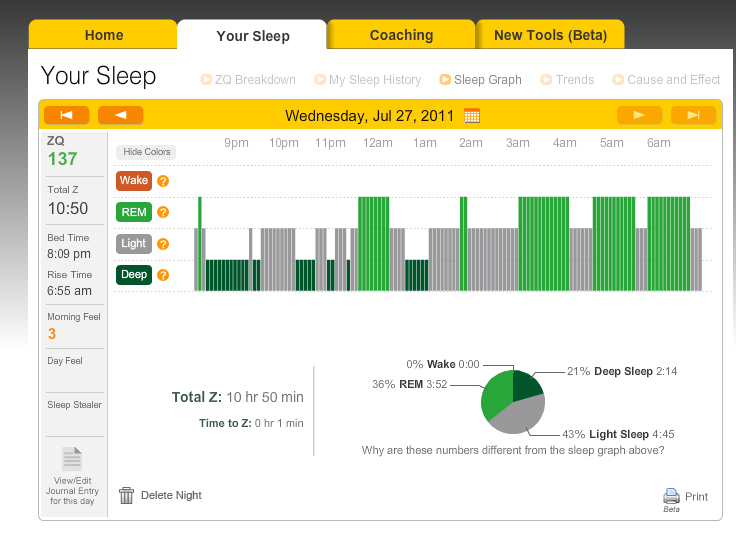
This just goes to show how important a good sleeping environment is!
Waking up in the night to turn the air-conditioning on for some cool air and white noise was a far cry from scavenging around for dry wood in the cold wet night although the white noise of the nearby river and stream at our camp the previous night was vastly more impressive than the hum of the hotel air-conditioning...
... and it is that sort of natural feature that made me want to do this again but this time be better prepared. It was all very well reading about this sort of thing but it's another to actually try it. I'd made the transition from "Armchair Wild Camper" to a real life Wild Camper and wasn't going to give up now. After making a reasonable attempt the first time I decided to give it another go and put in place some of the things that I'd learned the hard way from the first night. So re-energised I removed some kit that I didn't use and packed some other things that I thought would be useful (including a sleeping bag and Trangia stove) then on my own at a new location nearer home set up my shelter in a more enclosed way.
Remembering the slug / snail trail, it occurred to me that the CPAP and battery combination may need a sleeping bag / hammock of its own. If it did nothing more than keep them slime-free then it would be worth it but it may also help with the problem of them accumulating a layer of morning dew by keeping them off the cold groundsheet.
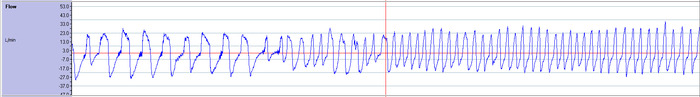
I was concerned that whatever method I used would still need to enable decent airflow to the CPAP so I put the battery, adapter and CPAP into a string "turtle" bag and suspended it from the ridge line using a caribina but this could also have been achieved using a decent knot (something that is a real test of how tight you are able to make the ridge line because although the S9 is light, the power brick and battery aren't).
In this photo I've lowered the side of my shelter to make the bag easier to see...
The string bag worked well because it allowed a good airflow and I was able to feed the CPAP hose through one of the holes in the bag. The bag was able to be moved along the line so that it was in a good position for when I went to sleep (not directly above my head, and not too near the edge of the shelter).
The bag helped a fair bit with the dew problem, although to be fair the weather conditions and my shelter weren't the same.
It would also be possible to wrap the CPAP / Battery combo in a lightweight towel before putting it into the bag as long as you were careful not to obstruct the air-intake of the CPAP.
It's also worth mentioning that it would be prudent to leave the CPAP machine safely tucked away until the smoke from your fire has subsided, otherwise every breath you take will smell of campfire smoke!
I'll definitely do this again. As far as my bushcraft skills go, I've got a lot to learn but as far as the CPAP is concerned I'm very happy with how things went and have proved to myself that being tethered to a machine at night shouldn't put a limitation on activities like this.
 Hypnagogia Blog
Hypnagogia Blog