REM Rebound
Looking back at my post about Sleep Debt, it seems illogical to me that I can be carrying round a lifetime's worth of sleep debt...
Why on the December 1st graph, didn't my brain arrange for all the debt to be paid back in one night, why do I not have solid nights of REM or SWS to catch up on all the lost sleep of my life?
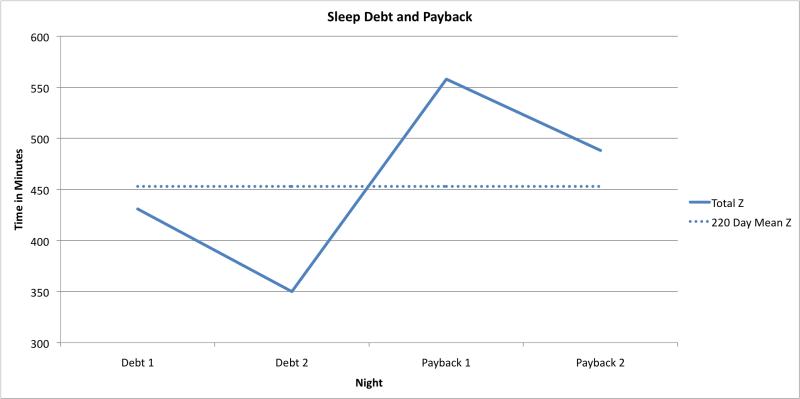
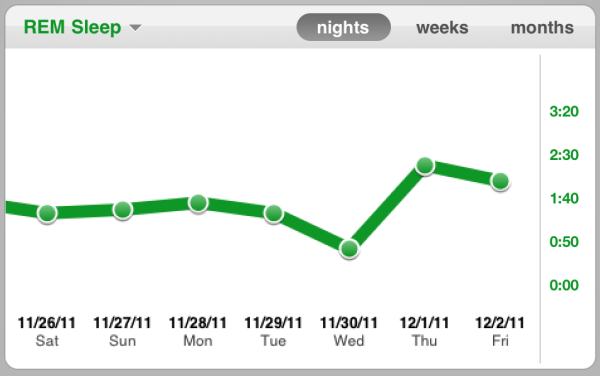
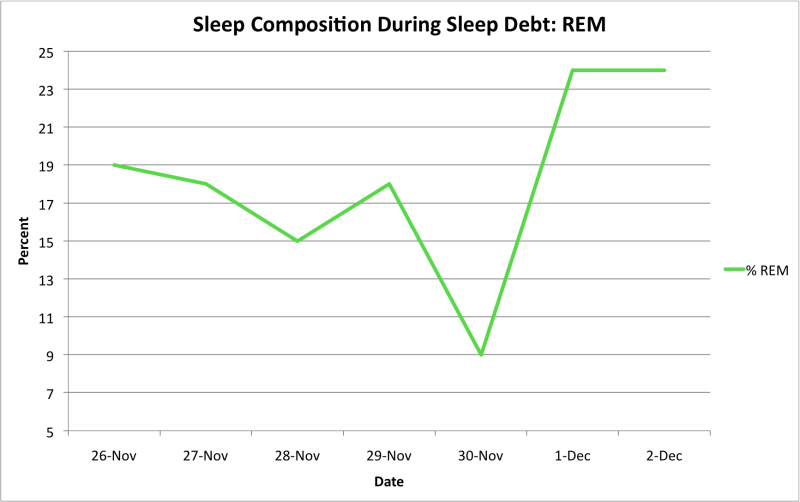
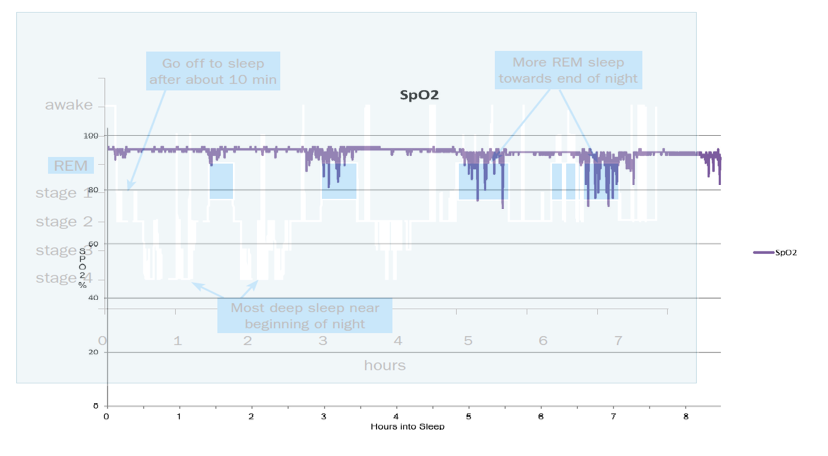
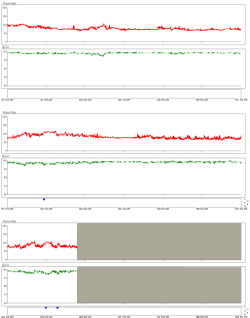
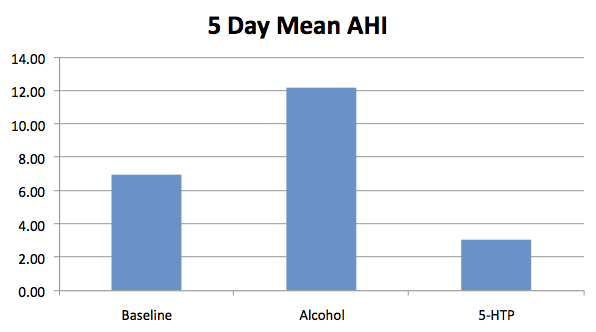
It's clear to see from the following graph that I roughly caught up on the REM sleep that I missed out on, the area below the mean REM on the debt days is roughly equal to the area above the mean on the payback days.
In fact the figues bear this out too. Assuming that my 220 day mean figure of 99 minutes is my desired amount then on the two debt days I lost 73 minutes of REM, 60 of which I caught up on over the two payback days.
Why don't we just have a night of "super concentrated sleep" without any (N1 or N2) to help us catch up on REM and slow-wave sleep?
Maybe light sleep (N1 and N2) also serves a purpose and is desirable to the body, hence it makes sure it has some each night, maybe the body actually needs N1 and N2 as a vehicle for REM and slow-wave sleep.
Maybe REM and slow-wave sleep don't need to be paid back on on a minute-by-minute basis.
From looking at the many nights of data that I have, I think it seems clear that I generally get my "normal" amount of slow-wave sleep, and that my issue is more with REM.
Perhaps each of us has an optimal amount of REM and more than that is unnecessary, perhaps it serves a function such as recharging the immune system or cognitive functions and their respective batteries can only be fully charged and no more. There is no point in over-charging a battery, so the body doesn't waste energy trying. Maybe the brain says "Okay, your immunity was low for a day, you were sluggish in thought too, you even dipped into your reserves, so we'll top you up with 'premium' rather than 'regular' tonight"
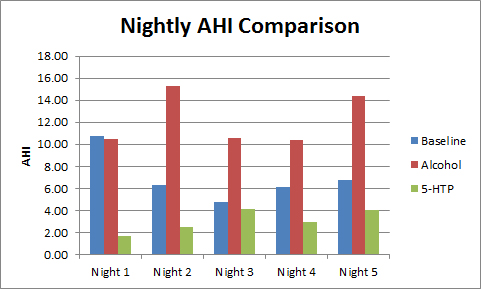
This is bourn out by this graph of the 13 nights where I had more than 140 minutes of REM sleep...
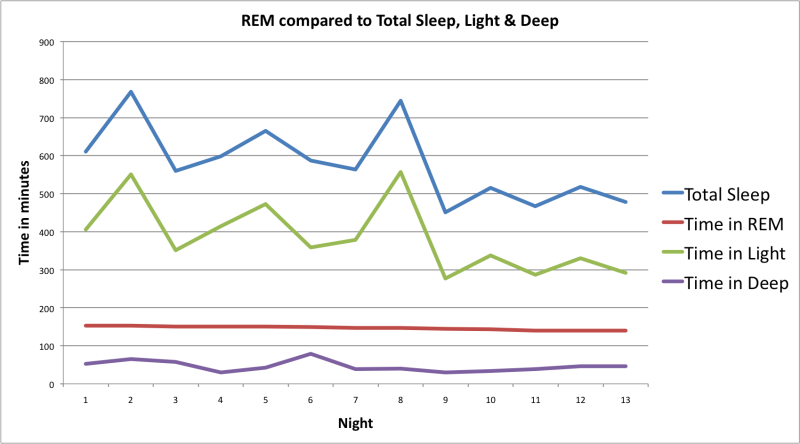
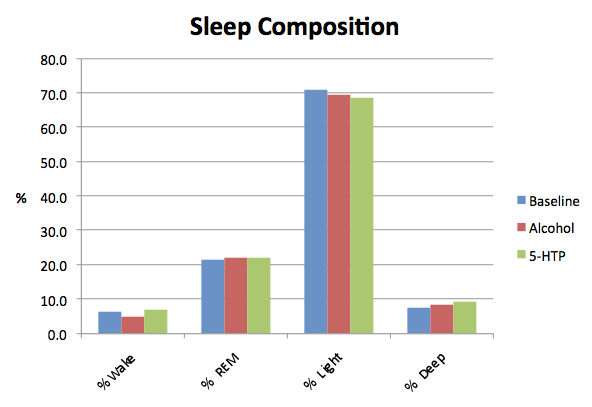
So, by selection, there is little change in the amount of REM (140 - 153) but there is a large variation in Light (N1 + N2) and Deep (Slow-wave) sleep. This shows something else besides total sleep time governs the amount of REM that the brain desires.
Yes, the total amount of sleep and REM can't be completely independent of each other because the total REM cannot exceed the total sleep, and the brain must also arrange time for slow-wave sleep too, but this suggests that if the brain desired more REM then it could arrange for a night of the "concentrated sleep" that I spoke of in the post about "Sleep Debt"
That describes conventional REM Rebound. However, as I said above I doubt that one is able to get more than a pre-set maximum amount of REM (which will vary for each person).
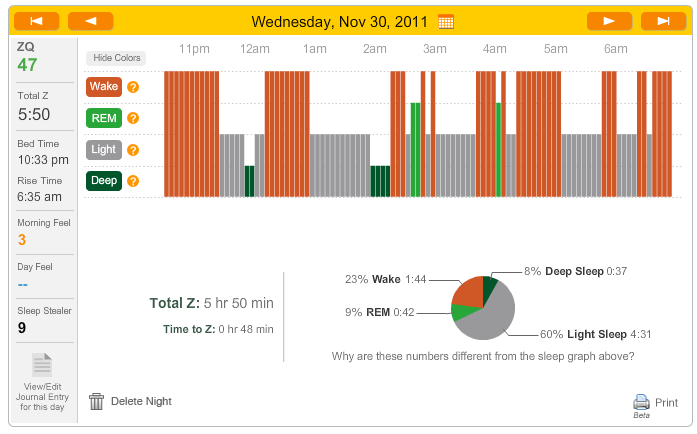
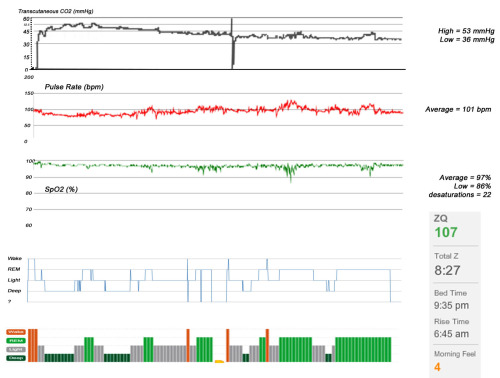
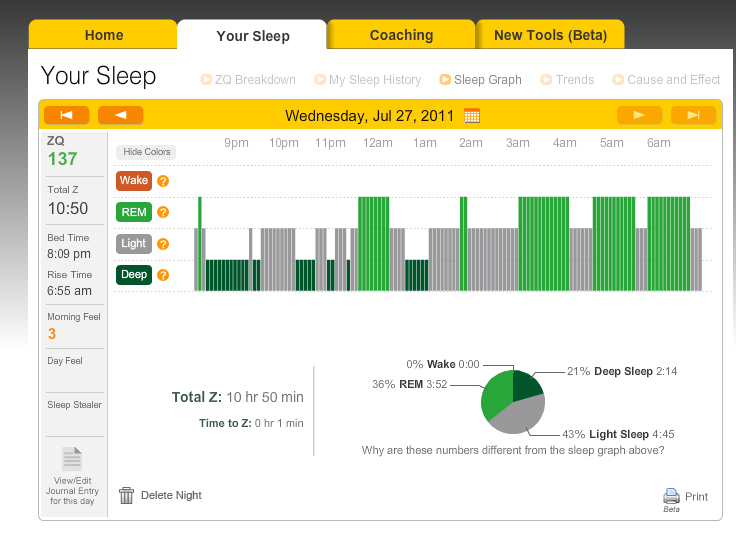
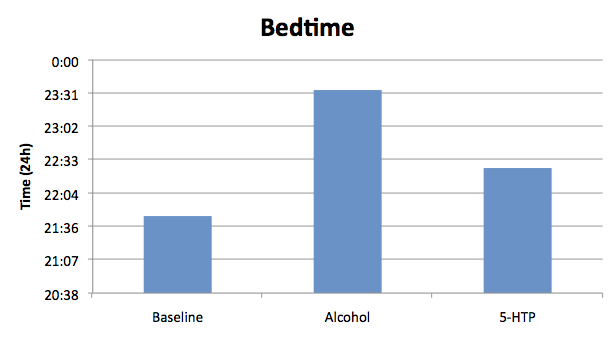
I think that the weekend of the Zeo Sleep Challenge goes some way to show this.
The idea was to have a competition where the highest sleep score (ZQ) wins. The ZQ isn't the same as "Sleep efficiency", it can be made higher by the length of time that you sleep. So my idea was to partially deprive myself of sleep for the two nights leading up to it and hope that I caught up on them for the night of the challenge.
I thought that I'd also help my chances by depriving myself of REM sleep during the time that I actually spent asleep, causing more REM to be necessary on the challenge night, hence a higher score because Zeo awards bonus points for REM and slow-wave sleep. In essence I was hoping to make use of "REM Rebound".
William Dement did this with students who volunteered in his early work in the lab. He used an EEG to determine when they were in REM sleep. As soon as he saw evidence of REM he woke them. Then let them go back to sleep until he saw another REM period. Needless to say this annoyed many of the volunteers, and some gave up.
How could I manage to do this without employing someone to watch over me?
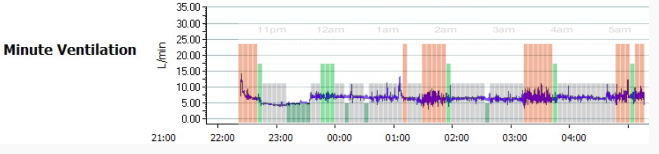
There is an excellent piece of software called ZeoScope that has been written by a Zeo user, Dan.
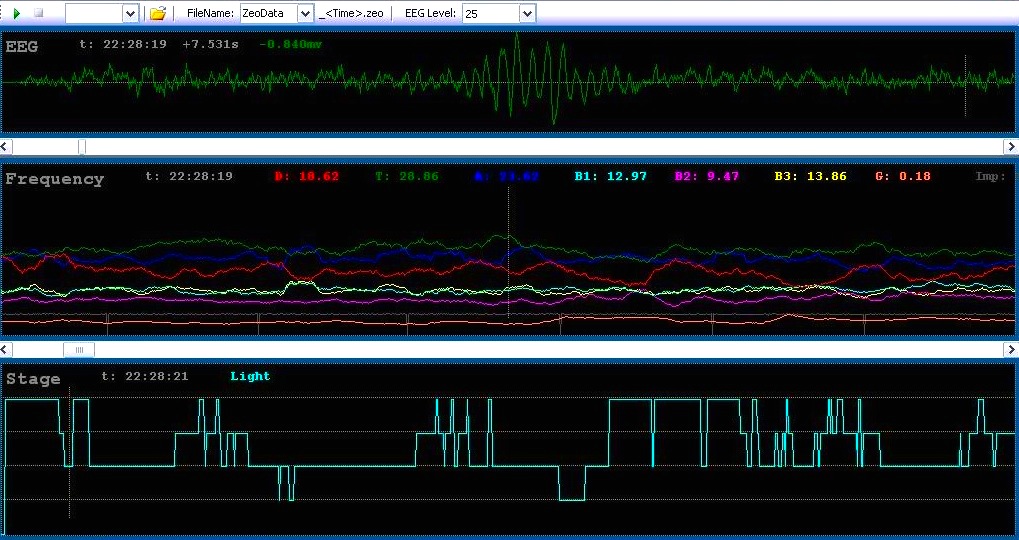
It was designed to work with the Zeo Raw Data Library, so that it receives the data from the Zeo and displays it on a PC. He also added in a function where the software can sound an audio alert when you have been in a certain sleep phase for a given period of time.
The purpose of this is to use as a trigger for a lucid dream (a dream in which the dreamer knows that they are dreaming and can consciously control the dream as if they were both the author and main character of the story).
It works well for this, if you select a nice quiet tone, such as raindrops or a soft voice telling you that you are dreaming.
I found a loud alarm clock tone and set it to play after I had 2 minutes of REM. I chose the alarm clock sound because I didn’t want to have a sound that I would ignore and incorporate into the dream.
After a couple of hours things seemed okay and I’d only been woken a couple of times, but as the night wore on the sounds became more frequent and persistent until I got annoyed and chose to get up early.
It was like being ripped out of another world, only to realise that you are in your bed and flapping an arm around trying to silence a non-existent alarm clock!
If I nodded off again quickly then I went straight back into REM and was greeted by an alarm again, so I quickly worked out that it was better to make sure that I was fully awake before going back to sleep.
It got to the point that as the flashing colours and shapes of dozing (hypnagogia) began to form coherent images the alarm would sound. Once I began to lucidly dream and remember thinking "Oh, I'm somewhere new... anytime now it'll go off..." and it did.
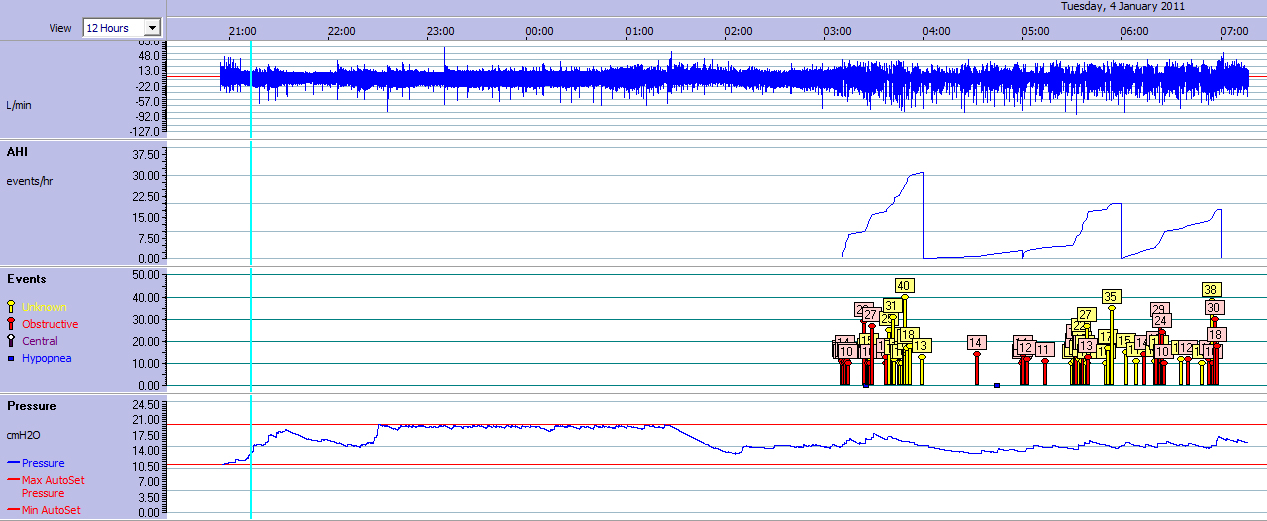
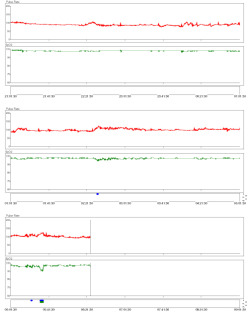
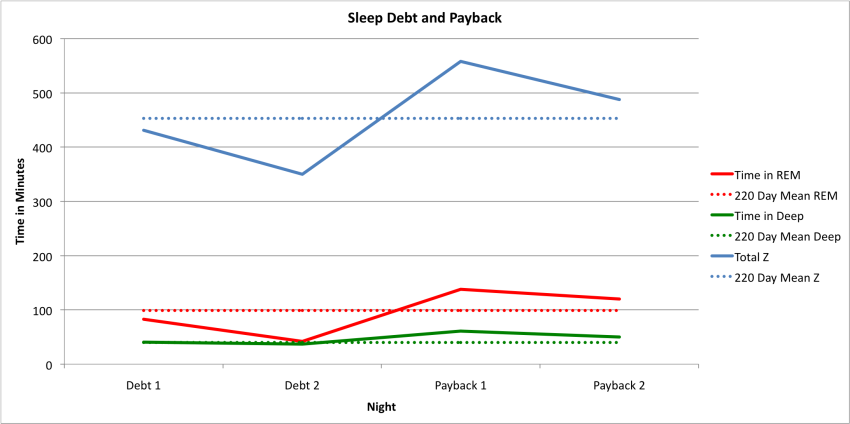
It turned out to be pretty effective...
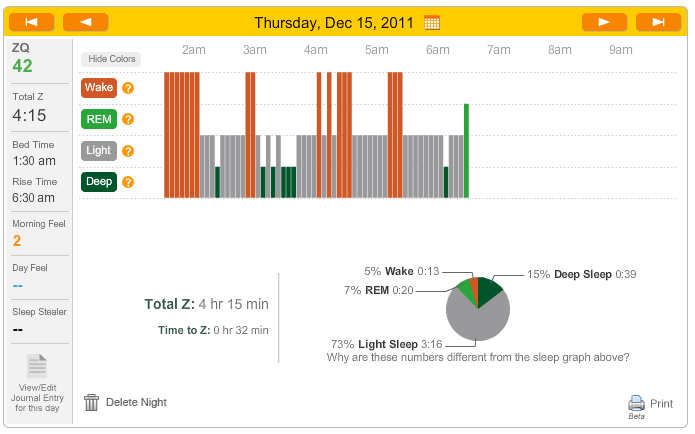
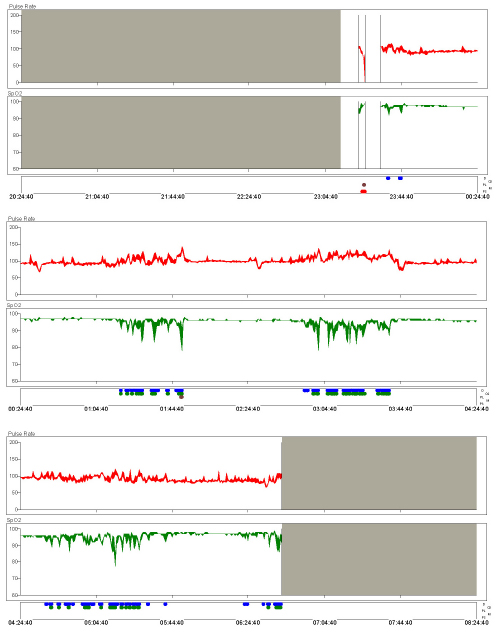
I only clocked up 20 minutes of REM compared to my usual 1 hour and 40 minutes – mission accomplished!
I attempted to deprive myself of REM for the following night.
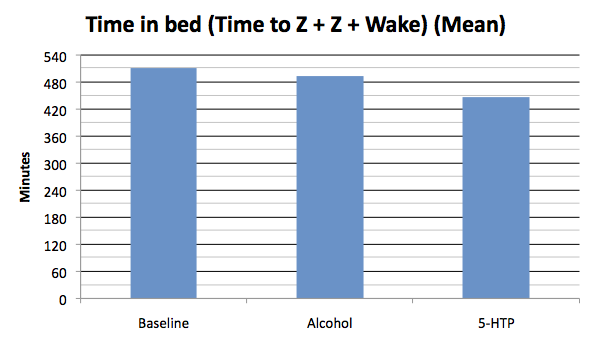
I slept for longer that night and ended up with 40 minutes of REM, still an hour short of my usual amount. So if the hour-for-an-hour payback idea is correct then I would owe 2:20h of REM, which means that on the night of the challenge, all being well I'd end up with 2:20h plus my normal amount of 1:40h giving a total of 4h REM.
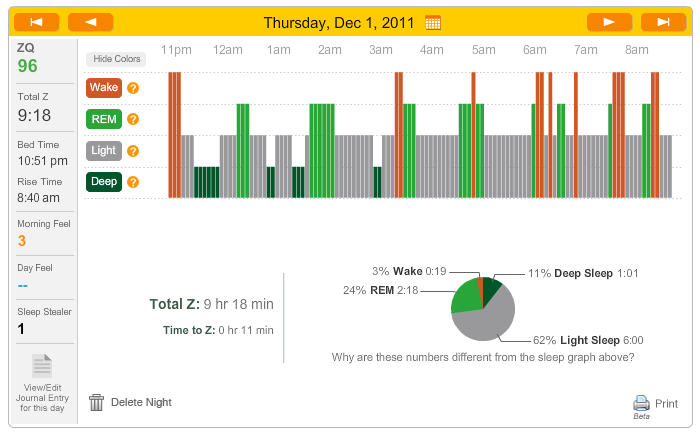
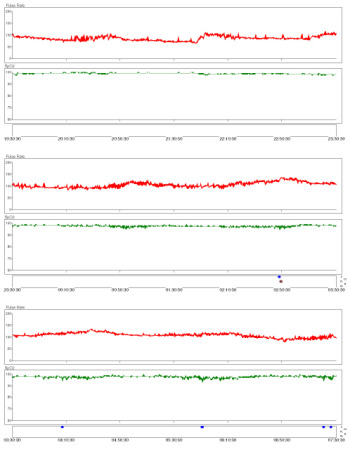
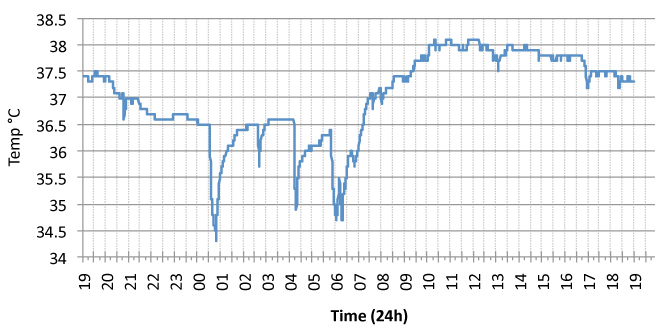
...but it didn't work out that way. In fact I had to force myself to stay asleep. I did manage to sleep for nearly 13 hours, but as you can see from the graph it was mainly filled with the "padding" of light sleep (N1 and N2).
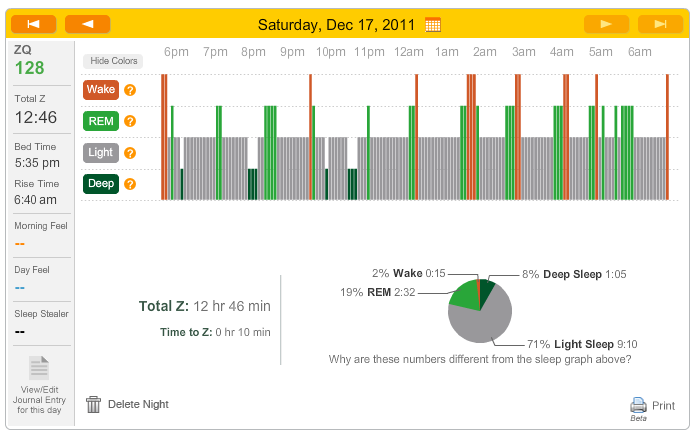
Compared to the hospital-payback night shown above I slept for 3:30h more, but only achieved 4 minutes additional deep sleep and 14 minutes additional REM. No one can say that I didn't give my body a chance to catch up on it's life long debt, and it failed to even catch up on the REM that it lost during the preceding two days.
Where is my missing REM?
Will I ever get it back?
Surely I gave my body enough chance to catch up on some much needed REM? Why did it squander the chance by filling the night with light sleep (N1 & N2)?
William Dement suggests that payback occurs over the course of many nights. That fits with my "hospital debt" being largely paid back over two nights. He recommends a period of a few weeks where you have no obligation to stay up late, or be forced awake by an alarm clock. Then after paying back the debt, your sleep will normalise into a pattern that is right for you.
I am torn between the conventional wisdom and what I experience firsthand. Perhaps the only way to reconcile them is that my awakenings during REM are the problem.
I guess that I am trying both approaches: sorting out the cause of my REM interuptions and trying to schedule my day in a way that is more friendly towards sleep.
Maybe one day I'll have a week of solid REM.
 Dement,
Dement,  REM,
REM,  REM Rebound,
REM Rebound,  Sleep Debt,
Sleep Debt,  sleep stage | in
sleep stage | in  Experiment,
Experiment,  Explanations
Explanations