Apnoeas, me? My Baseline AHI
I'm going to be exploring some of the sensible and not so sensible suggestions in order to bring down my AHI (see my post "What is an Apnoea?" for an explanation).
To do that I needed reliable data, so I decided on a 5 day mean with a few basic rules:
- No coffee after 3pm
- Monday - Friday monitoring only (to ensure routine sleep and wake times)
- No alcohol
- No other supplements known to affect sleep
- Begin sleep on my back (supine)
- Motion detection IR camera (for verification of events if needed)
- The same apnoea / hypopnea scoring criteria will be used throughout
I could use the IR camera to detect sleep position, but that would take a lot more time, so until I have a system that can detect that reliably then I won't include that data, and I may re-evaluate some weeks using that ability.
I did initially check the camera to see if I attempted to breathe when the system was detecting apnoeas. I did make some respiratory effort, so I will make the presumption (for now) that my apnoeas are obstructive in nature.
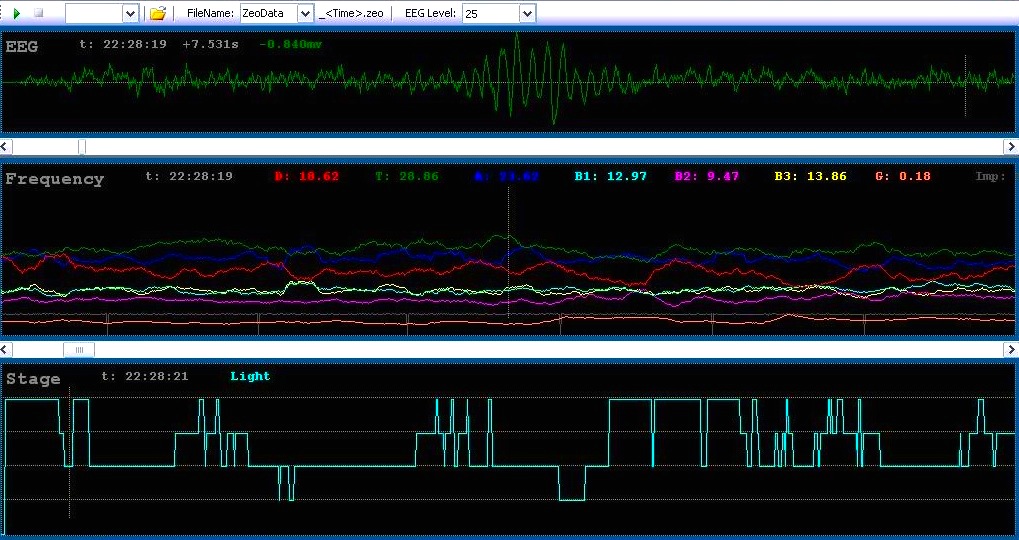
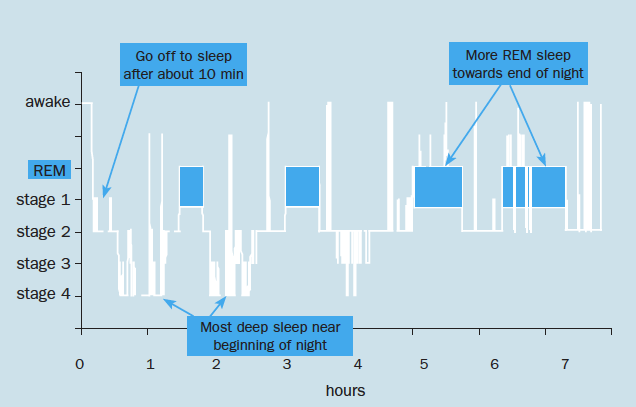
I also noticed that when the oxygen desaturations due to apnoeas were compared to the Zeo hypnogram, that like my son's, they were clustered around REM sleep.
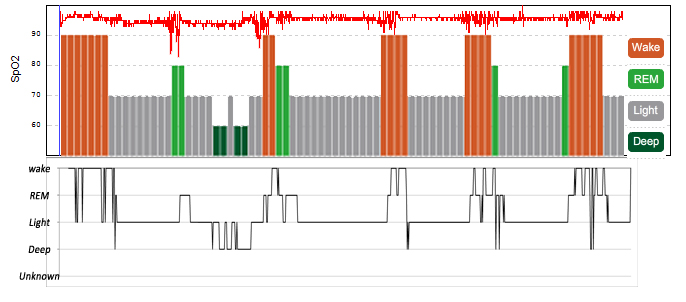
The top line is my oxygen level.
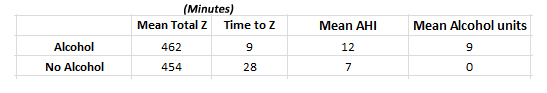
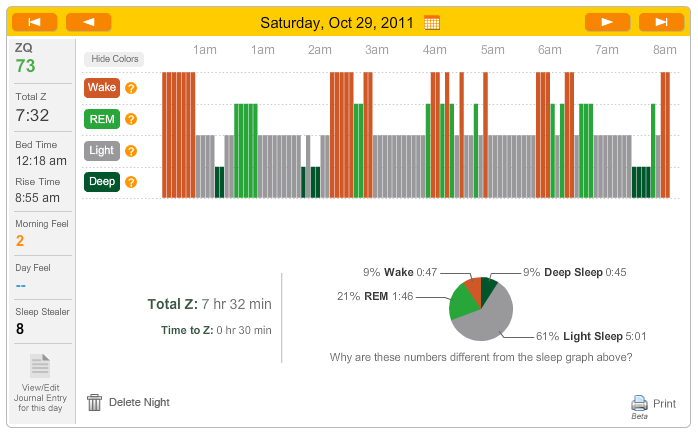
It does look like I'm awake for those periods, but the black line is a more detailed Zeo hypnogram (data calculated on a 30 second basis). Zeo has a scoring system and shows the highest scoring sleep stage as being the dominant one. "Wake" scores the highest; this makes sense, as being awake is probably the most important thing to show when you are supposed to be sleeping.
The 30 second graph shows why the main Zeo graph shows a lot of wakefulness during the night... I have oxygen desaturations which in turn wake me up, hence Zeo shows "wakefulness for the whole 5 minute epoch. However, when you see Zeo's calculations of time spent in each sleep stage, these are based on the more detailed 30 second data.
Sleep apnoea can run in families. Whether that is a factor or not, my diagnosis (albeit a self-diagnosis) doesn't surprise me. I sometimes snore, I wake up with headache a lot, and I could do with losing a bit of weight.
I have long suffered with sleep paralysis, and I suspect that being disturbed in REM sleep is a major factor in that, if not the sole cause.
So, how is this a problem?
My average AHI (number of apnoeas and hypopneas per hour) is 7, hence I am classified as having "Mild Obstructive Sleep Apnoea".
The classification ranges are:
<5 - Normal (unless symptomatic)
5-15 - Mild
15-30 - Moderate
30+ - Severe
The REM element brings the name to "Mild REM-Related Obstructive Sleep Apnoea"
I will say that this "diagnosis" is an amateur one, it may not correlate with a professional one in a sleep lab, but if I use the same equipment throughout this experiment the results will still be valid, just relative to my original numbers.
So, what if I don't want to have that diagnosis, what if I want to be "normal" (says the man who sleeps with electrodes on his head, prongs up his nose and a camera watching him)?
Standard advice:
- Lose weight if you are overweight (even a small amount can make a difference)
That's all very well, and something that I will do, but that won't help me fix my sleep tonight will it?
Other advice includes:
- Prop the head of your bed up by 4-6 of inches (takes the weight off your neck)
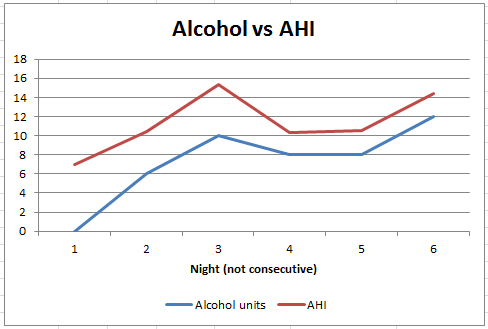
- Cut down on alcohol (see this blog entry on alcohol)
- Quit smoking
- Use a mandibular advancement device (pushes the bottom jaw forward to hold the airway open)
- Use a CPAP device (see this blog entry on NIV)
- Avoid caffeine and heavy meals within two hours of bed
- Use a nasal dilator (keeps the nostrils open)
- Try a nasal saline spray
- Throat exercises
- Surgery
I'll evaluate some of these (plus a few more ideas that I have) and back up the findings with a 5 day mean AHI and sleep graphs.
Let's face it, we're all looking for quick-fix solutions, and I'm not trying to cut corners, but I am trying to help myself whilst on the journey to losing a bit of weight.
So that I don't confuse the issue I will not intentionally lose weight until I have tried some of the other methods.
So, in essence I am looking for some way of bringing my AHI down, along with the time that I spend awake at night.
...but before I do that, how about trying to INCREASE my AHI? Next blog post.
 REM,
REM,  apnoea,
apnoea,  baseline | in
baseline | in  Apnoea,
Apnoea,  Experiment
Experiment